|
|
Official Journal of the
|
ISSN: 1983-991X
|
|
| Original Article « PDF file » |
|
Accessory Spleen Detection at Laparoscopic Splenectomy is Adequate for Immune Thrombocytopenic Purpura - a Prospective Study
Doralice Mariá Leite Batista, MD1; Fernanda Silva Guedes, MD1; Antonio Carlos de Barros Lima Jr, MD1; Eduardo Kanaan, MD2; Marcos Filgueiras, MD3; Ricardo Zorron, MD, MSc, PhD4
1 Department of Surgery, University Hospital Teresopolis HCTCO-FESO, Rio de Janeiro, Brazil; 2 Chairman, Division of General Surgery, Hospital Municipal Lourenço Jorge, Rio de Janeiro, Brazil; 3 Professor, Department of Surgery, University Hospital Teresopolis HCTCO-FESO, Rio de Janeiro, Brazil; 4 Professor and Chairman, Department of Surgery, University Hospital Teresopolis HCTCO-FESO, Rio de Janeiro, Brazil. Research performed at Division of General Surgery, Hospital Municipal Lourenço Jorge, Rio de Janeiro, Brazil.
ABSTRACT
Objectives: Accessory spleens are foci of splenic tissue found commonly adjacent to the main spleen. Incidence ranges from 10 to 20% in general population. However, they occur with a higher frequency in patients with hematologic diseases. Immune Thrombocytopenic Purpura (ITP) stands out amongst these illnesses, and a detailed identification of these foci is extremely necessary to guarantee the therapeutic success. According to these data, the present study aims to analyze the effectiveness of laparoscopy in investigating the presence of accessories spleens. Methods: Thirty-seven patients with hematologic disease and indication for elective splenectomy underwent videolaparoscopy splenectomy, and they were documented prospectively. The technique preconized right lateral decubitus position and the use of three trocars. Results: The accessory spleen was found in eleven cases, what means 29.7% (11/37). However, neither the TC, nor the USG was capable to detect its presence in none of these cases where it was present. Eight patients (21.6%) needed transfusion during the surgery or postoperative period. The average length of hospital stay was of 2.41 days (varying of 2 to 6 days). The patients had been seen regularly in ambulatory, having an average follow-up time of 12.9 months. Of the 37 patients with ITP, 27 (72.9%) had satisfactory response with significant increase of platelets. No death, as well as major complications occurred. Conclusions: The data obtained in this study shows that laparoscopic splenectomy allows high accuracy for detection of accessory spleens and consequently, high rates of success in promoting permanent and complete remission of ITP.
Key words: immune thrombocytopenic purpura, ITP, accessory spleen, laparoscopy, laparoscopic splenectomy.
Bras. J. Video-Sur, 2008, v. 1, n. 4: 156-162
| Accepted after revision: September, 02, 2008. |
INTRODUCTION
ccessory spleens are foci of splenic tissue found
commonly adjacent to the main spleen.
This phenomenon elapses of alterations in the
embryologic development during the fifth week of intrauterine
life. 1,8 Incidence ranges from 5 to 10% in
general population. However, they occur with a
higher frequency in patients with hematologic
diseases. 9, 16, 36, 58, 59 Immune thrombocytopenic purpura (ITP)
stands out amongst these illnesses, and a detailed
identification of these foci is extremely necessary to guarantee
the therapeutic success. 16, 19, 23, 35, 47, 52.
ITP is an auto-immune disorder that promotes an accelerated phagocytosis of platelets by
the reticuloendothelial system, mainly in the spleen.
It frequently manifests with spontaneous bleeding.
ITP affects both children and adults, with
different manifestations and evolution. In children, it
typically presents with the sudden onset of petechiae and
has a favorable outcome. In the meanwhile, ITP in
adults occurs with insidious onset and trends to become
a chronic disease. 3, 8, 14, 18, 41
The diagnosis of immune thrombocytopenic purpura is an exclusion diagnosis. It must be
moved away secondary causes, like forms in association
with systemic erythematosus, the antiphospholipid
syndrome, immunodeficiency states, lymphoproliferative
disorders, infections like immunodeficiency virus and hepatitis
C virus and therapy with drugs such as heparin and
quinidine. 1,8, 46 In adults patients, treatment praises
the use of oral prednisone (1.0-1.5 mg/kg/d), mainly in
the acute forms. Another therapeutics agents like azatioprine and cyclophosphamide are also
indicated. Nevertheless, rates of complete and draw
out remission with drugs are low (around 25%). By contrast, splenectomy promotes permanent
remission in more than 70% of the cases, becoming the
treatment of choice. 1, 4, 11, 15, 23, 27, 32, 41, 44, 46
Laparoscopic access for splenectomy was first performed by Delaitre
11 and Maignen 11 in 1991. Since then, laparoscopic techniques has been
preferred for resulting in less postoperative pain, reduced
degree of respiratory function, reduced length of hospital
stay and earlier return to daily activities. 5, 14, 20, 38, 39,44, 50
Several studies suggest that laparoscopy also produces less inflammatory response to surgical
trauma when compared to conventional splenectomy.
In addition, complications after the laparoscopic procedure are less common and complex. The
main complications described are cerotic
collections, intrabdominal hematoma and pleural
effusion. However, complications such as hepatic
abscess, bleeding and pulmonary embolism are more
frequent in conventional procedures. 2, 4, 7, 23, 28, 30, 32, 33, 50
In spite of the innumerable advantages of
videolaparoscopy, factors such as surgeons' experience, spleen's
size and obesity restrict the effectiveness of the splenectomy .
20, 37, 40, 46, 51
Amongst the cases of failure in surgical treatment, it is described the finding of
functional splenic tissue due to the presence of
accessory spleen. Nowadays, surgeons dispose of
Computed Tomography (CT) and Scintilography for
pre-operative identification of these structures. However, both exams may fail, so it is crucial
that the surgeon pursues accessories spleens during
the surgical act. 19, 35, 11, 15 According to these data,
the present study aims to analyze the effectiveness
of laparoscopy in investigating the presence of accessories spleens.
METHODS
During a 5-year period, 37 patients with hematologic disease and indication for elective splenectomy underwent surgery at Hospital Municipal Lourenço Jorge and Hospital das Clínicas de Teresópolis (HCTCO-FESO), Rio de Janeiro and they were prospectively documented. The standardization of the technique with completely lateral approach, using three trocars, bipolar coagulation and simple nonabsorbable ligatures spared the use of endoclips, vascular staplers and alternative energy sources, and it was the pattern of the procedure.
Surgical Technique
The patient is placed in full right lateral decubitus position setting the body in
jack-knife position and 15º Tredenlemburg. Vesical
and orogastric catheters are placed. Surgeon and
first auxiliary (camera) place themselves in front of
the patient, while the equipment stays on the back of
the patient. 12
An incision of 1cm is made in the line of left nipple, about 10 cm under the costal margin, to
insert the first trocar. Reaching the peritoneum, repair
wires are placed in order to avoid leakage and allow
the placement of a 10 mm trocar that is placed
under direct vision. The pneumoperitoneum was
created through this 10 mm trocar, always using pressure
of less than 12 mmHg, in order to prevent metabolic
and hemodynamic changes. Another 10 mm trocar was placed 10 cm to the right of the first trocar,
often corresponding to the medium axilar line.
Scissors, bipolar scalpel, aspirator and endoclips are
used preferably by this port, as well as the withdrawal
of the specimen, after enlargement of the incision
from 2 to 3 cm. The third trocar (5 mm) was placed
below and to the right from xyphoid appendix, serving to
the left-hand instrument of the surgeon.
After the trocars were placed, adhesiolysis was made. Even if the patient did not have
previous history of surgery this step is necessary, in order
to detach splenic flexure, and avoid inadvertent
injuries by electric current. A detailed investigation
is made, delimitating the presence of accessory spleens, as well as concurrent abnormalities.
The inspection starts at the jejunum and ileum,
passing to the transverse colon, mesentery, stomach,
shorts vessels, splenocolic ligament and splenic hilum,
the three last ones correspond to the most frequent
sites (Figure 1A-1D). Accessory spleens were found
in 31.8% of our casuistic, they had been dried up
at the beginning of the surgery, before the
extraction of the organ. In most cases, the tissue's
extraction (spleen and accessory spleen) has
succeeded through the 10 mm trocar, using sealed plastic
bag easily found in supermarkets
(ZiplocTM) and sterilized through ethylene oxide process.
Fascial closure of 10mm wounds were performed
using Vicryl 0. Patients were given oral intake on the
same operative day.
 |
 |
 |
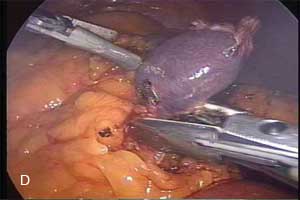 |
| Figure 1 - Common sites of accessory spleens found at laparoscopic splenectomy for ITP. 1A. Inferior polar artery location. 1B. Splenic hilum. 1C. Major omentum. 1D. Splenocolonic attachment. | |
RESULTS
Accessory spleens were found in eleven cases, which means 29.7% (11/37). However,
neither preoperative ultrasonography was capable to
detect their presence in none of these cases where they
were present, nor preoperative CT could report
their presence in only one case (6cm accessory
spleen). Of these, 3 had been found next to the inferior
polar artery, one next to the short gastric vessels, two
next to splenic hylum and one in the larger omentum.
The greatest of them, 6 cm of diameter, was
removed together with the spleen at the end of the surgery.
It was necessary an additional 5 mm trocar in 8
patients (20.52%), usually in the left flank, allowing
best exposition of the superior pole of the spleen.
Eight patients (21.6%) needed blood transfusion during the surgery or in the
postoperative period. These patients represent cases where it
was necessary to stabilize low platelets during
the procedure when an intense bleeding occurred,
even when using electrocoagulation and careful
dissection. Mean estimated blood loss was 98.25 ml, varying
from 20 to 400 ml, in which the highest loss of blood
(400ml) was the only case of conversion in the casuistic.
In this case, after the control of all the vessels and
complete mobilization of the organ, the untied region
kept blood; therefore, it was necessary conversion
to achieve hemostasis. This patient also failed the
clinical response of splenectomy to control ITP, keeping
low platelets even with elevated doses of steroids.
Three patients suffered laceration of capsule during the surgery. In two cases there was rupture
of the plastic bag, thus another bag was necessary
with new positioning of the spleen for its extraction.
Both patients had good evolution during the
postoperative time. The average length of hospital stay was
2.41 days (varying of 2 to 6 days). The patients had
been seen regularly in ambulatory, with an average
follow-up time of 12.9 months. Of the 37 patients with
ITP, 27 (72.9%) had satisfactory response with
significant increase of platelets.
Fewer complications occurred in 6 of 37 patients (16.2%). Two patients
developed subcutaneous hematoma on the left flank,
with spontaneous resolution, one of them presented
small pleural effusion that did not need draining, another
one developed with fecaloma on the fourth
postoperative day. A patient developed pain on left flank 18
months after surgery, the presence of remaining spleen
tissue was diagnosed by CT scan, but with complete
remission of ITP, the patient was submitted to open
surgery. The last patient with lumbar pain 26 months
after surgery underwent a CT exam that revealed a pancreatic tail pseudocyst, which was
treated conservatively. Neither infection of the wound
nor pneumonia due to the procedure was observed. It
was not observed death, as well as major complications.
DISCUSSION
Many aspects of understanding spleen disease have changed since KAZNELSON,
a medical student from Praga, reported for the
first time a therapeutic splenectomy for ITP in 1916
26. The advent of minimum invasive surgery,
and thereupon its application for splenectomy by DELAITRE e MAIGNIEN
11 in 1991 have resulted in the necessity to increase casuistry and
prospective studies to establish the real role of the
method. Descriptions of initial experiences have
been published by DEXTER e cols.13, LEFOR e
cols.31, ZORNIG e cols.57 e PHILIPS e
cols.40, among others, showing the feasibility and safety of
the method, little by little replacing open surgery
mainly in big centers with higher numbers of
patients. Nowadays, this procedure represents the
golden standard method for hematologic disease's
treatment with indication to splenectomy.
GAGNER 17 has instituted lateral
decubitus and lateral approach as a routine for
videolaparoscopic adrenalectomy, which smoothed away difficulties
for identifying and dissecting the structures in adrenalectomy, as well as in splenectomy when
this knowledge was applied by other surgeons 21, 27, 43,
47. TRIAS 54 has compared the lateral approach to
the anterior approach, emphasizing the advantages of
the first one that allows shorter the operative time as
well as numbers of trocars. The position in lateral
decubitus made spleen pendency possible due to gravity, thus
it was not necessary great manipulation of the
organ and removal of adjacent organs. Placing the patient
in this way makes the use of two additional trocars
not necessary.
The possibility to perform videolaparoscopic splenectomy using only three trocars was
proposed initially by GOSSOT 21, SZOLD 48 and TRIAS
54, with few changes of positioning and approach,
but always using laparoscopic vascular staplers
6, 10, 59 In our experience, great part of the vessels were
stamped by bipolar electrocoagulation, the splenic hilum
was criteriously sectioned after performing a double tie
with nonabsorbable wire (polypropylene) through knot
or suture. Operative bleeding did not occur. None of
the patients were submitted to another surgery
because of postoperative bleeding.
Accessory spleens are found in 10% of general population, besides in patients with
hematologic diseases these congenital abnormalities could
be detected in 30% of the cases which were
submitted to splenectomy. 8, 18, 35, 58
In some ITP cases, to not locate these structures may result in splenosis
and failure of the surgical therapeutic. Hence it
follows that complete removal of splenic tissue is
essential, and for this a diligent inventory in searching the
splenic tissue must be made as a routine before
beginning dissection. The splenic hilum, major and
minor omentum and splenocolic ligaments can be
effectively evaluated. An adequate investigation must disclose
any ectopic splenic tissue. In our casuistry, the
rate detection was of 29.7%.
Computed Tomography (CT) does not seem mandatory for pre-operative detection of
accessory spleen. Typically, these structures appears as
delimited and small masses (< 2cm) with homogeneous
aspect to the contrasted exam. MORTELE et al have
shown that the most frequent location of accessory spleen
is: postero-medial spleen zone, antero-lateral zone
near the superior pole of left kidney and lateral,
superior and posterior zones of the tail of the pancreas.
GIGOT and cols. in study a comparing per operative CT
and Scintilography with laparoscopic exploration
reported that both exams can detect accessory spleens in
25% of the cases, while laparoscopic investigation
shows an accuracy of 75% in detection of accessory spleens.
STANECK 45 and cols have mentioned
an identification rate of 43% with CT, and they
have assigned this increase to the use of equipment
with higher resolution.
CT and Scintilography are crucial for the identification of these abnormalities, although they
are less accurate than the laparoscopic approach. Therefore, several authors have reported an
increased difficulty in identifying accessory spleens during
the surgery, when these were not demonstrated by
imaging exams. 19, 36, 47, 52
Despite these unsatisfactory rates of preoperative detection, the laparoscopic inventory
is decisive to assure that any residual splenic
tissue persists after splenectomy.
TARGARONA 50 and SZOLD 47
have reported that the "main-point" to assure
identification by laparoscopic approach is excising the
accessory tissue before performing the splenectomy.
These authors have shown that an identification of
accessory spleens is easier when the anatomy is
preserved. PARK 38 and cols affirm that the lateral
approach could be harmful in the identification of
accessory tissue, a time that this technique would make
difficult the access to the places where these
abnormalities more frequently occur. However, our experience
does not corroborate such affirmation, and other
approaches have been deferred due to the several advantages
that have already been exposed with splenectomy in
the lateral decubitus position. 17, 21, 27, 49, 53, 55, 56
Some studies have reported higher rate of detection through conventional splenectomy. In
our opinion, there is no sense in preferring
conventional surgery even if these data were true. However,
we stand out that many other studies does not
support this affirmation; therefore, it is doubtful to
attribute this advantage to conventional surgery.
19, 36, 52
CONCLUSIONS
Laparoscopic splenectomy has become the procedure of choice for elective splenectomy
because of their feasibility and safety. Compared to
the conventional technique, videolaparoscopy presents
less morbidity rate, less postoperative pain, reduce
length of hospital stay and fast return to daily
activities. Despite of the several advantages of
videolaparoscopy, some factors such as surgeons' experience,
spleen's size and obesity restrict the effectiveness of
the splenectomy. Several studies report that ITP is
the most frequent indication for elective splenectomy,
and in 20% of these patients accessory spleens are present.
Detection of accessory spleens is still a challenge for surgeons, and it certainly is the
main cause of failure in the surgical treatment for
ITP. Improvements are necessary to reach better
rates of identification of this embryologic
disorder. However, several data demonstrate that unquestionably videolaparoscopy is the way to
reach this objective.
REFERENCES
1. Akwari OE, Itani KMF, Coleman RE, et al.
Splenectomy for primary and recurrent immune
thrombocytopenic purpura (ITP): Current criteria for patient selection
and results. Ann Surg 1987; 206: 529.
2. Balagué C, Targarona E, Vela S, Alonso V, García A, Pey
A, Leija C, garriga J, Trias M. Esplenectomía
Laparoscópica: resultados a largo plazo de uma serie prospectiva de
260 pacientes em funcíon del diagnóstico
hematológico. Associación Mexicana de Cirurgía Endoscópica , 2004. Vol
5 nº 1, 5:11
3. Bearnes S, Emil S, Kosi M, Applebaum H, Atkinson J.
A comparison of laparoscopic versus open splenectomy
in children. Am Surg 1995; 61: 908-910.
4. Brodsky JA, Brody FJ, Walsch RM, Malm JÁ, Ponsky
JL. Laparoscopic splenectomy: experience with 100 cases.
Surg Endosc 2002; 16: 851-854.
5. Brunt LM, Langer JC, Quasebarth MA, et al.
Comparative analysis of laparoscopic versus open splenectomy. Am
J Surg 1996; 172: 596.
6. Cardenás A, Millán JP. Esplenectomia laparoscópica com
3 trocáres: Experiência inicial. Associación Mexicana de
Cirurgía Endoscópica , 2004. Vol 5 nº 3, 131:133
7. Chand B, Walsh RM, Ponsky J, Brody F.
Pancreatic complications following laparoscopic splenectomy.
Surg Endosc 2001; 15: 1273-1276.
8. Cines D, Blanchette VS. Immune trombocytopenic
purpura. New england Journal of medicine, 2002. Vol 346, nº13, march.
9. Coelho JC, Claus CM, Bombana B, Machuca TN,
Sobottka WH. Esplenectomia laparoscópica. Revista do Colégio
Brasileiro de Cirurgiões, 2004. Vol 31, nº 3: 200-203
10. Corcione F, Esposito C, Cuccurullo D, Settembre A,
Miranda L, Capasso P, Piccolboni D. Technical standartization
of laparoscopic splenectomy:experience with 105 cases.
Surg Endosc 2002; 16: 972-974.
11. Delaitre B, Maignien B. Splenectomie par
voie coelioscopique: 1 observation. Presse Med 1991; 20: 2263.
12. Delaitre B. Laparoscopic splenectomy: the "hanged
spleen" technique. Surg Endosc 1995; 9: 528-529.
13. Dexter SPL, Martin IG, Alao D, Norfolk DR,
MacMahon MJ. Laparoscopic splenectomy: the suspended
pedicle technique. Surg Endosc 1996; 10: 393-396.
14. Donini A, Baccarani U, Terrosu G, Corno V, Ermacora
A, Pasqualucci A, Bresadola F. Laparoscopic vs
open splenectomy in the management of hematologic
diseases. Surg Endosc 1999; 13: 1220-1225.
15. Duperxter T, Brody F, Felsher J, Walsh M, Rosen M,
Ponsky J. Predictive Factors for Successful
laparoscopic Splenectomy in patientes with Immune
Thrombocytopenic Purpura. Arch Surgery, 2004. Vol 139.
16. Flowers JL, Lefor AT, Steers J, et al.
Laparoscopic splenectomy in patients with hematologic diseases. Ann
Surg 1996; 224:19.
17. Gagner M, et al. Laparoscopic adrenalectomy:
the importance of a flank approach in the lateral
decubitus position. Surg Endosc 1994; 8: 135-138.
18. Gigot JF, de Goyet JV, Van Beers BE, et al.
Laparoscopic splenectomy in adults and children: Experience with
31 patients. Surgery 1996; 119:384.
19. Gigot JF, Jamar F, Ferrant A, et al. Inadequate detection
of accessory spleens and splenosis with
laparoscopic splenectomy: A shortcoming of the laparoscopic
approach in hematologic diseases. Surg Endosc 1998; 12: 101-106.
20. Glasgow RE, Yee LF, Mulvihil SJ.
Laparoscopic splenectomy: the emerging standard. Surg Endosc 1997;
11; 108-112.
21. Gossot D, Fritsch S, Célérier M. Laparoscopic
splenectomy: Optimal vascular control using the lateral approach
and ultrassonic dissection. Surg Endosc 1999; 13: 21-25.
22. Gründel K, Böhm B, Bauwens K, Junghans T, Zorrón
RS. Influence of acute hemorrhage and pneumoperitoneum
on hemodynamic and respiratory parameters. Surg Endosc
1998; 12: 809-812.
23. Haschizume M, Ohta M, Kishihara F, Kawanaka
H, Tomikawa M, Ueno K, Tanoue K, Higashi H, Kitano
S, Sugimachi K. Laparoscopic splenectomy for
idiopathic thrombocytopenic purpura: comparison of
laparoscopic surgery and conventional open surgery. Surg Laparosc
Endosc 1996; 6: 129-135.
24. Heniford BT, Matthews BD, Sing RF, Backus C, Pratt
B, Greene FL. Initial results with an electrothermal bipolar
vessel sealer. Surg Endosc 2001; 15: 799-801
25. Junghans T, Böhm B, Zorrón RS , Schwenk W. Effects of
induced intravenous helium and CO2 embolism on
the cardiovascular system. Minimal Invasive Chirurgie 1999;
8: 52-56.
26. Kaznelson P. Verschwinden der häemorragischen
diathese bei einem falle von essentieller thrombopenie (frank)
nach Milzextirpation: Splenogene thrombolytische Purpura.
Wien Klin Wochenschr 1916; 29; 1451-1454.
27. Kathouda N, Grant SW, Mavor E, Friedlander MH,
Lord RV, Achanta K, Essani R, Mason R. Predictors of
response after laparoscopic splenectomy for immune thrombocytopenic purpura. Surg Endosc 2001; 15: 484-488.
28. Kathouda N, Hurwitz MB, Rivera RT, et al.
Laparoscopic splenectomy: Outcome and efficacy in 103
consecutive patients. Ann Surg 1998; 228: 568.
29. Kennedy JS, Stranaham PL, Taylor KD, Chandler JG.
High burst strength, feedback-controlled bipolar vessel
sealing. Surg Endosc 1998; 12: 876-878.
30. Kumar RJ, Borzi PA. Splenosis in a port site
after laparoscopic splenectomy. Surg Endosc 2001; 413-414.
31. Lefor AT, Melvin WS, Bailey RW, Flowers JL.
Laparoscopic splenectomy in the management of
immune thrombocytopenic purpura. Surgery 1993; 114: 613-618.
32. Lozano-Salazar RR, Herrera MF, Vargas-Vorackova
F, Loopez-Karpovitch X. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Am
J Surg 1998; 176: 366-369.
33. Mac Rae HM, Yakimets WW, Reynolds T.
Perioperative complications of splenectomy for hematologic disease.
Can J Surg 1992; 35: 432.
34. Marassi A, Vignali A, Zuliani W, Biguzzi E, Bergamo
C, Gianotti L, Di Carlo V. Splenectomy for
idiopathic thrombocytopenic purpura: comparison of laparoscopic
and conventional surgery. Surg Endosc 1999; 13: 17-20.
35. Morris KT, Horvath KD, Jobe BA, Swanstrom
LL. Laparoscopic management of accessory spleens in
immune thrombocytopenic purpura. Surg Endosc 1999; 13: 520-522.
36. Mortelé KJ, Mortelé B, Silverman SG. CT Features of
the Accessory Spleen. American Journal of Radiology,
2004. 183:1653_1657
37. Pace DE, Chiasson PM, Schlachta CM, Mamazza J,
Poulin EC. Laparoscopic splenectomy: does the training
of minimally invasive surgical fellows affect outcomes?
Surg Endosc 2002; 16: 954-956.
38. Park A, Marcaccio M, Strenbach M, Witzke D,
Fitzgerald. Laparoscopic vs Open Splenectomy. Arch Surgery,
1999. Vol 134.
39. Park A, Birgisson G, Mastrangelo MJ, Marcaccio MJ,
Witzke DB. Laparoscopic splenectomy: outcomes and
lessons learned from over 200 cases. Surgery 2000; 128: 660-667.
40. Philips E, Carroll B, Fallas M. Laparoscopic
splenectomy. Surg Endosc 1994; 8 : 931-933.
41. Rogers J, Yousuf A., Kleinhaus S. Laparoscopic
accessory splenectomy in recurrent chronic immune
thrombocytopenic purpura. Surg laparosc Endosc 1997; 7: 83-85.
42. Rosen M, Brody F, Walsch RM, Tarnoff M, Malm J,
Ponsky J. Outcome of laparoscopic splenectomy based
on hematologic indication. Surg Endosc 2002; 16: 272-279.
43. Santos MM, Zorrón RS, Toaspern TV, Lino T, Kanaan
E. Esplenectomia Vídeo-laparoscópica: Aspectos
Técnicos. (ABS) Revista de Cirurgia Vídeoendoscópica 2002; 5(3): 96.
44. Shimomatsuya T, Horiuchi T. Laparoscopic
splenectomy for treatment of patients with idiopathic
thrombocytopenic purpura: comparison with open splenectomy. Surg
Endosc 1999; 13: 563-566.
45. Stanek A, Stefaniak T, Makarewicz W, Kaska L,
Podg_rczyk H, Hellman A, Lachinski A. Accessory spleens:
preoperative diagnostics limitations and operational strategy
in laparoscopic approach to splenectomy in
idiopathic thrombocytopenic purpura patients. Langenbecks
Arch Surgery, 2005, 390:47_51
46. Stanton CJ. Laparoscopic splenectomy for
idiopathic thrombocytopenic purpura (ITP): a five-year
experience. Surg Endosc 1999; 13: 1083-1086.
47. Szold A, Kamat M, Nadu A, Eldor A. Laparoscopic
accessory splenectomy for recurrent idiopathic
thrombocytopenic purpura and hemolytic anemia. Surg Endosc 2000; 14:
761-763.
48. Szold A, Sagi B, Merhav H, Klausner JM.
Optimizing laparoscopic splenectomy: technical details and
experience in 59 patients. Surg Endosc 1998; 12: 1078-1081.
49. Tanoue K, Okita K, Akahoshi T, Konishi K, Gotoh
N, Tsutsumi N, Tomikawa M, Hashizume M.
Laparoscopic splenectomy for hematologic diseases. Surgery 2002;
131: 318-323.
50. Targarona EM, Espert JJ, Bombuy E, Vidal O, Cerdan
G, Artigas V, Trias M. Complications of
laparoscopic Splenectomy. Arch Surgery, 2000. Vol 135.
51. Targarona EM, Espert JJ, Cerdán G, Balagué C, Piulachs
J, Sugrañes G, Artigas V, Trias M. Effect of spleen size
on splenectomy outcome: a comparison of open and laparoscopic surgery. Surg Endosc 1999; 13: 559-562.
52. Targarona EM, Espert JJ, Cerdán G, Balagué C,,
Sugrañes G, Ayuso C, Lomeña F, Bosch F, Trias M. Residual
Splenic Function After laparoscopic Splenectomy. Arch
Surgery, 1998. Vol 133.
53. Torelli P, Cavaliere D, Casaccia M, Panaro F, Grondona
P, Rossi E, Santini G, Truini M, Gobbi M, Bacigalupo A,
Valente U. Laparoscopic splenectomy for
hematological diseases. Surg Endosc 2002; 16: 965-971.
54. Trias M, Targarona EM, Espert JJ, Balagué C.
Laparoscopic surgery for splenic disorders: lessons learned from a
series of 64 cases. Surg Endosc 1998; 12: 66-72.
55. Trias M, Targarona EM, Espert JJ, Cerdan G, Bombuy
E, Vidal O, Artigas V. Impact of hematological diagnosis
on early and late outcome after laparoscopic splenectomy:
an analysis of 111 cases. Surg Endosc 2000; 14: 556-560.
56. Watson D, Coventry B, Chin T, Gill G, Malycha
P. Laparoscopic versus open splenectomy for immune thrombocytopenic purpura. Surgery 1997; 121: 18-22.
57. Zornig C, Emmermann A, Peiper M, Zschaber R,
Broelsch CE. Laparoskopische Splenektomie. Chirurg 1993;
64(4): 314-316.
58. Zorrón RS, Neto SH, Kanaan E, Toaspern TV, Chaves
LP, Filho DM. Esplenectomia vídeo-laparoscópica para
púrpura trombocitopênica imune: técnica e resultados. Revista
do Colégio Brasileiro de Cirurgiões, 2004. Vol 31. nº 4, 265:270.
59. Zorrón RS, Neto SH, Kanaan E, Toaspern TV.
Esplenectomia Videolaparoscópica: Padronização técnica com Três
Trocartes e Ligadura Hilar. Revista Brasileira de Videocirugia, 2003.
Correspondence address:
Prof. Ricardo Zorron
Department of Surgery
University Hospital Teresopolis HCTCO-FESO
Email: rzorron@terra.com.br