|
|
Official Journal of the
|
ISSN: 1983-991X
|
|
| Original Article « PDF file » |
|
Mechanical Bowel Preparation for Laparoscopic Surgery in Pigs - A Pilot Study
William Kondo1; José Belarmino da Gama Filho2; Gabriela Silva Uchôa2; Marcelo Imbuzeiro Cores2; Paulo Henrique Candido de Carvalho2;Paula Marina Brito Jorge2; Ana Carolina Assunção Progana2; Paulo Guimarães3
1 General Surgeon, trainer at the 23rd Gynecologic Laparoscopy Course (Brasília, 2008); 2 Veterinary Physician at the 23rd Gynecologic Laparoscopy Course (Brasília, 2008); 3 Gynecologist, coordinator at the 23rd Gynecologic Laparoscopy Course (Brasília, 2008).
ABSTRACT
Objectives: Mechanical bowel preparation (MBP) is performed routinely before several gynecologic surgeries to
reduce the risk of postoperative infectious complications and to improve the surgical field. Nevertheless, the available
medical literature is not able to demonstrate any benefit of this procedure and some authors even report deleterious outcomes
in patients undergoing bowel preparation, with increased rates of septic complications, anastomotic leakages and
surgical site infections. The aim of this pilot study is to evaluate three different types of MBP for laparoscopic in an
experimental model. Material and Methods: Twenty female pigs were randomized into 4 groups to preoperative MBP (sodium
phosphate, glycerin or manitol) or surgery without MBP. During surgery, the pneumoperitoneum was inflated using Veress
needle puncture at the supra-umbilical region and the 10mm trocar was positioned for the zero degree laparoscope.
The abdominal cavity was inspected and the status of the bowel preparation was checked by three different
surgeons. Results: The MBP could be done in all pigs using an orogastric tube. One pig did not undergo the laparoscopic
procedure because it died after the MBP with manitol. One pig of the glycerin group had an intestinal perforation by the Veress
needle and it was excluded from the final analysis. According to the surgeons' analysis, MBP using sodium phosphate
and glycerin presented the best quality of surgical field, the former being the best one.
Conclusions: According to this pilot study, the sodium phosphate seems to be the best way to perform MBP in pigs.
Key words: mechanical bowel preparation, colo-rectal surgery, gynecologic laparoscopy.
Bras. J. Video-Sur, 2008, v. 1, n. 4: 144-149
| Accepted after revision: July, 07, 2008. |
INTRODUCTION
echanical bowel preparation (MBP) is routinely
used by many surgeons before several gynecologic surgeries, either for benign or
malign conditions. The rationale for its use would be
to decrease the peritoneal contamination in case
of iatrogenic injury and empty the bowel of its
contents to improve both surgical field visualization and
handling of the bowel1.
Recently the necessity of using bowel preparation as a routine has been questioned by
several surgical subspecialties, including
urologic2 and colorectal
surgery3-7. Some randomized studies performed in elective colorectal surgery have
shown no benefit in bowel preparation in the prognosis
of these procedures5,7, while other studies even
suggest that mechanical bowel preparation may be
harmful, with higher rates of septic complications,
anastomotic dehiscence and surgical wound
infection3,4,6.
Literature about mechanical bowel preparation in gynecologic surgery is still
insufficient. MUZII and cols.8 compared patients that
underwent diagnostic or operative laparoscopy with or
without bowel preparation with sodium phosphate, it was
not observed any difference in quality of the surgical
field and handling of the bowel. The operative time
and complications rate were similar in both
groups, supporting the idea that bowel preparation does
not facilitate the surgery. Moreover, bowel
preparation increases patient discomfort the night before
the surgery (insomnia, weakness, abdominal
distention, hunger/thirst and nausea/vomiting), and neither
the postoperative discomfort nor the length of hospital
stay are modified.
The objective of this study is to evaluate
three different types of bowel preparation for
laparoscopic surgery in a porcine experimental model in relation
to the ability to improve the surgical field and to
facilitate bowel handling.
METHODS
This study was performed during a training course in gynecologic laparoscopic surgery in
May 2008 using tricoss pigs (Landrace, Large White
and Duroc breed), from pig farms with sanitary control
by the Ministry of Agriculture, vaccinated and fed
with balanced diet according to the pigs age.
Twenty female pigs weighing from 12 to 18 kg were used. They were randomly divided in 4
groups of 5 animals each as follows:
· Group 1: control group that did not
received any bowel preparation;
· Group 2: bowel preparation with 50 ml of sodium phosphate;
· Group 3: bowel preparation with 50 ml of glycerin;
· Group 4: bowel preparation with 125 ml
of 20% mannitol solution.
All animals accomplished 12 hours of fasting before the surgical procedure. Animals of groups 2,
3 and 4 received bowel preparation through lavage
with an orogastric tube number 12 (Figure 1) after anesthesia using intramuscular ketamine(15mg/kg).
 |
Figure 1 - Orograstric tube insertion to perform bowel preparation. |
Veterinarian team performed the anesthesia using endovenous infusion with 200 mg of
ketamine, 0,4ml of xylazine 2% and 20mg of diazepam
diluted in 16,6 ml of isotonic saline solution. The control
of the anesthetic plan was based on the evaluation
of the corneal-palpebral reflex, respiratory and
heart rates.
After the animal was placed in appropriated surgical table (Figure 2), it was performed the
puncture of the Veress needle at the supraumbilical region
to insufflate de abdominal cavity with carbon dioxide
to a pressure of 10mmHg. The first 10mm trocar was blinded inserted and a zero-degree optical system
was inserted to investigate the abdominal cavity.
 |
Figure 2 - Placement of the animal on the surgical table. |
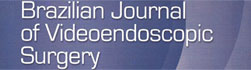
The analysis of the bowel loops was individually performed by three different
surgeons based on the degree system depicted in table 1,
without previously knowing the method of bowel
preparation that was used. After evaluation of each surgeon,
it was chosen the most voted result. In case of
three different opinions the surgeons went back to
the surgery room to reach a consensus.
 |
After the procedure, the animals remained in observation in a postoperative ward where
they received nourishment and antibiotics. These
animals were sent back to the swine farm two days after
the procedure.
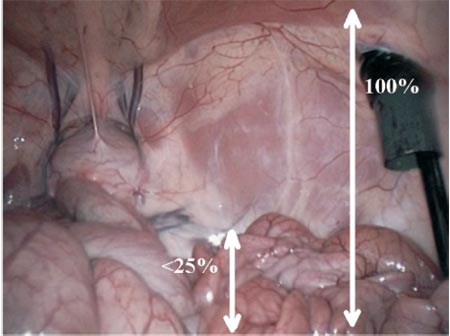 |
Figure3 - Excellent bowel preparation. |
 |
Figure 4 -Good bowel preparation. |
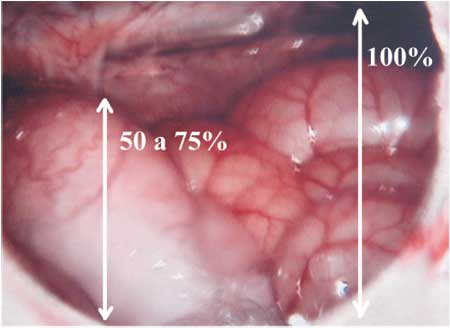 |
Figure 5 - Regular bowel preparation. |
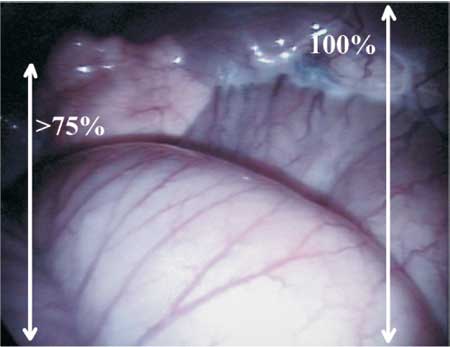 |
Figure 6 - Poor bowel preparation. |
RESULTS
Bowel preparation was possible in all of the animals as they were under the effect of
ketamine; therefore, medication was administered through
an orogastric tube.
Of the 20 animals included in this study,
only 19 animals were submitted to surgery in view of
a death caused by the depletion of the
extracellular space as the bowel preparation was done
with mannitol.
During the surgical procedure there was a case of complication in one animal that received
bowel preparation with glycerin. There was bowel perforation caused by the Veress needle
insufflating carbon dioxide into the small bowel loop. The
injured area was identified and sutured; however, this
animal was excluded from our study. Consequently, of the
20 animals selected for the study, only 18 were
included in the final analysis.
Table 2 depicted the evaluation of small and large bowel loops and the global evaluation
in accordance with the type of bowel preparation used. Groups 2 and 3 depicted less distension
of the bowel loop and better quality of the
surgical field in the evaluation of the surgeons, in
which the best group the one prepared with sodium phosphate. In the group treated with mannitol
it was observed a higher incidence of bowel distension, even when compared with the
group that did not received any preparation.
 |
DISCUSSION
Mechanical bowel preparation is used to: (1) remove the bulky intraluminal contents to improve
the surgical field visualization and to facilitate the
handling of the bowel and (2) decrease peritoneal and
wound contamination by the intraluminal content in case of
bowel opening1. The former argument is true for
any intra-abdominal surgical procedure, mainly the laparoscopic ones in which carbon dioxide
insufflation compete for the same space of the bowel
loops. Therefore, theoretically, mechanical bowel
preparation could decrease stool and gas content, reducing
the volume of bowel intraluminal contents and
ameliorating the surgical field. The second justification,
however, is only true for cases of iatrogenic bowel injury
or complicated cases (advanced or recurrent
cancer, radiotherapy complications and some benign gynelogical conditions such as severe
endometriosis, severe adhesions, pelvic abscess and ovarian
remnant syndrome in which bowel opening can be
anticipated9,10. The other gynecological
procedures have a low incidence of bowel
injury9,10.
Few studies about bowel preparation in gynecologic surgery are available in the
literature. However, the result obtained with randomized
studies in elective colorectal surgery may be extrapolated
to gynecologic surgery in which iatrogenic bowel
injury occur.
BROWNSON and cols.4 compared 179 patients submitted to elective colorectal surgery
with or without bowel preparation using PEG (polyethylene glycole). It was observed 5,8%
of wound infections in patients receiving bowel preparation and 7,5% in patients receiving no
bowel preparation (p is not significant). The rate
of intrabdominal sepsis (9.3%, vs. 2.2%)and the
rate of anastomotic leakage (11.9%, vs. 1.5%) were significantly higher in the bowel preparation
group. The conclusion of this study was that bowel preparation using PEG does not reduce the rate
of septic complications of colorectal surgery, and
may even be detrimental. In a randomized study
published in 1994, Burke et al. 5 compared 169
patients submitted to elective colorectal surgery
receiving bowel preparation using sodium picosulfate 10
mg and patients receiving no bowel preparation.
The overall morbidity rate was 18% in both groups
(p is not significant). Anastomosis leakage rates were
similar in both groups of patients. The authors concluded that mechanical bowel preparation
does not influence the prognosis of elective
colorectal surgery. SANTOS and cols.6 randomized 149
patients admitted for elective colorectal surgery in two
groups (bowel preparation using laxatives and enemas
versus no bowel preparation), it was observed the
incidence of wound infection was significantly higher in
the bowel preparation group. The incidence of anastomotic dehiscences in the bowel
preparation group was 10% and in the no bowel preparation
group was 5%. OLIVEIRA and cols.11 compared PEG
and NaP (sodium phosphate) administered
preoperatively to 200 patients submitted to elective
colorectal surgery. Patients who received PEG had
significantly more side effects. However, evaluation of
bowel cleansing in the intraoperative time revealed
no significant differences between the two
regimens. One anastomotic leak occurred in each group
(1% vs. 1%), whereas four septic complications
occurred in the PEG group (4%) versus 1 in the NaP
group (1%;p is not significant). The authors concluded
that the efficacy of PEG and NaP solutions was
similar; however, the NaP solution was, better tolerated.
In 2000, MIETTINEM and cols.7published
randomized study including 267 consecutive patients
submitted to elective colorectal surgery that received
either PEG or no bowel preparation. No difference
was observed in regard to anastomotic leaks (4% in
the PEG group vs. 2% in the control group) or in
other surgical site infections (6% vs. 5%). Median time
to restoration of normal bowel function and median postoperative hospital stay were similar in the
two groups. A metanalysis recently
published3 evaluated the role of mechanical bowel preparation in
reducing the risk of anastomotic leakages and other septic
or non-septic complications in 1454 patients
submitted to colorectal surgery. It was observed a higher
rate of anastomotic leakage in the mechanical
bowel preparation group (5,6% vs. 3,2%; p=0,032).
MUZII and cols.8 conducted a
prospective randomized study to evaluate the effect of
bowel preparation in patients that underwent
gynecologic laparoscopic surgery. The patients were divided in
2 groups (with or without preparation), thus the
night before surgery, the bowel preparation was
performed with 90ml of oral sodium phosphate. The next
morning, the intensity of different symptoms resulting from
the bowel preparation (insomnia, weakness,
abdominal distension, nausea and thirst, difficulty in drinking
the solution and overall discomfort) was evaluated with
a visual analogue scale and all the symptoms were significantly more severe in patients that
received bowel preparation. During surgery, it was not
observed any advantage regarding the improvement in
the surgical field visualization or handling of the
bowel loops comparing both groups. The operative
time, complications rates and subjective evaluation of
the procedure were similar in both groups. There was
no significant difference in regard to reduced postoperative discomfort and length of hospital stay.
The objective of our study was to evaluate three methods of bowel preparation in swine
that underwent gynecologic laparoscopic surgery. It
was only a pilot study to identify the best bowel
preparation method in female pigs that will enable us to
conduct other experimental studies comparing surgeries
with or without bowel preparation. In spite of the
limited number of animals used in each group our
results showed the sodium phosphate as the ideal
bowel preparation method in swine, since only this
substance was able to prepare the small and colon loops
with 100% of efficacy (good and excellent
results). Mannitol provided a regular bowel preparation in
most of the cases and caused the death of one animal
due to dehydration. Results with glycerin were good,
but in one case the bowel preparation was regular and
in other there was bowel perforation during the
Veress needle insertion which might have occurred due to
a bad bowel preparation or bad surgical technique.
CONCLUSIONS
Studies evaluating the role of bowel preparation in gynecologic surgeries are still
necessary in the literature. When we extrapolate the
results obtained in colorectal surgery studies, it was
observed that bowel preparation does not offer any
advantage in the intraoperative time or in the reduction
of postoperative complications, which could even
worsen the surgical outcomes. This pilot study evaluated
three bowel preparation methods in swine and our preliminary results seem to suggest that the
sodium phosphate could be the best method to bowel preparation in swine. Once the best bowel
preparation method in animal model is chosen we are
performing new experimental investigation to establish the
real role of bowel preparation in gynecologic
laparoscopic surgeries.
REFERENCES
1. Muzii L, Angioli R, Zullo MA, Calcagno M, Panici
PB. Bowel preparation for gynecological surgery. Crit Rev
Oncol Hematol. 2003; 48:311-5.
2. Shafii M, Murphy DM, Donovan MG, Hickey DP.
Is mechanical bowel preparation necessary in
patients undergoing cystectomy and urinary diversion? BJU Int.
2002; 89:879-81.
3. Slim K, Vicaut E, Panis Y, Chipponi J. Meta-analysis
of randomized clinical trials of colorectal surgery with or
without mechanical bowel preparation. Br J Surg. 2004; 91:1125-30.
4. Brownson P, Jenkins S, Nott D, Ellenbogen S.
Mechanical bowel preparation before colorectal surgery: results of
a postoperative randomized trial. Br J Surg 1992;79:461-2.
5. Burke P, Mealy K, Gillen P, Joyce W, Traynor O, Hyland
J. Requirement for bowel preparation in colorectal surgery.
Br J Surg. 1994;81:907-10.
6. Santos JC Jr, Batista J, Sirimarco MT, Guimarães AS,
Levy CE. Prospective randomized trial of mechanical
bowel preparation in patients undergoing elective colorectal
surgery. Br J Surg. 1994;81:1673-6.
7. Miettinen RP, Laitinen ST, Mäkelä JT, Pääkkönen
ME. Bowel preparation with oral polyethylene glycol
electrolyte solution vs. no preparation in elective open colorectal
surgery: prospective, randomized study. Dis Colon Rectum.
2000; 43:669-75.
8. Muzii L, Bellati F, Zullo MA, Manci N, Angioli R,
Panici PB. Mechanical bowel preparation before
gynecologic laparoscopy: a randomized, single-blind, controlled
trial. Fertil Steril. 2006; 85:689-93.
9. Johnston K, Rosen D, Cario G, Chou D, Carlton M,
Cooper M, et al. Major complications arising from 1265
operative laparoscopic cases: a prospective review from a single
center. J Minim Invasive Gynecol. 2007; 14:339-44.
10. Magrina JF. Complications of laparoscopic surgery.
Clin Obstet Gynecol. 2002; 45:469-80.
11. Oliveira L, Wexner SD, Daniel N, DeMarta D, Weiss
EG, Nogueras JJ, et al. Mechanical bowel preparation for
elective colorectal surgery. A prospective, randomized,
surgeon-blinded trial comparing sodium phosphate and
polyethylene glycol-based oral lavage solutions. Dis Colon Rectum.
1997; 40:585-91.
Correspondence address:
William Kondo
Endereço: Av. Getúlio Vargas, 3163 ap. 21
CEP 80240-041
Curitiba - Paraná
Email: williamkondo@yahoo.com