|
|
Official Journal of the
|
ISSN: 1983-991X
|
|
| Case Report « PDF file » |
|
Is Time Monitoring Necessary for Preventing Fluid Overload in Hysteroscopic Surgery?
Márlon de Freitas Fonseca, M.D., M.Sc., Ph.D.1; Claudio Moura Andrade Junior, M.D.2; Eduardo de Almeida Nogueira, M.D.3; Luiz Carlos da Silva Santos, M.D.4; Claudio Peixoto Crispi, M.D.5
1 Associate Professor of Gynecological Endoscopy Post-graduate Course and Physician Anesthesiologist, Instituto Fernandes Figueira, Fundação Oswaldo Cruz, Rio de Janeiro; Associate Researcher, Instituto de Biofísica Carlos Chagas Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brasil; 2 Associate Professor of Gynecological Endoscopy Post-graduate Course, Instituto Fernandes Figueira, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil; 3 Physician Instructor of Anesthesiology Post-graduate Program of Brazilian Society of Anesthesiology, Hospital Central da Polícia Militar, Rio de Janeiro, Brasil; 4 Associate Professor of Gynecological Endoscopy Post-graduate Course, Instituto Fernandes Figueira, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil; 5 Associate Professor and General Coordinator of Gynecological Endoscopy Post-graduate Course, Instituto Fernandes Figueira, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil.
ABSTRACT
This case report summarily describes pulmonary complications after saline overload in
hysteroscopic-laparoscopic multiple myomectomy and, finally, suggests a simple prophylactic strategy for fluid balance, not only increasing safety
but also allowing longer procedures when possible and necessary.
Key words: laparoscopic, colectomy, colorectal, cancer, preceptorship.
Bras. J. Video-Sur, 2008, v. 1, n. 3: 122-127
| Accepted after revision: June, 25, 2008. |
CASE REPORT
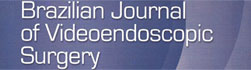
healthy 42-year-old woman was candidate to multiple myomectomy because excessive
menstrual bleeding and secondary iron deficiency (Figures
1A and 1B). Hysterectomy was not considered in
order to guarantee her reproductive status.
Hysteroscopic-laparoscopic approach under general anesthesia
with oral intubation was indicated. Saline (NaCl 0,9%)
was used as uterine distention media and the maximal
fluid pressure was adjusted to 100 mm Hg (Stryker Endoscopy Pump®).
A 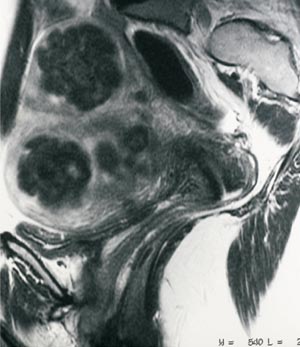 |
B  |
Figure 1 - Pelvis and myomatous uterus view through
nuclear magnetic resonance; A: lateral view; B: axial view. |
|
After 12 minutes of hysteroscopic myomectomy with bipolar electrosurgery system
(Figure 2), the patient presented gradual increase
in airway pressure, decrease in oxygen saturation
and wheezing, suggesting bronchospasm. After
checking anesthetic and clinical conditions, fluid balance
was made while surgery was interrupted because of iatrogenic acute pulmonary edema. Impressively,
it was noticed a difference of 4.500 mL of saline.
Without delay, it was administered 100% oxygen,
intravenously morphine 6 mg and furosemide 60 mg, positive
end-expiratory pressure was adjusted to 5-10 cm
H20 and the condition became close to normal in 30
minutes. Fortunately, distension media was not a
non-electrolytic solution as, for example, sorbitol and manitol
which probably would have generated most
serious consequences. The cause of the massive
saline absorption was initially attributed to the high
flow device (wash button) which was exceptionally
pressed several times in order to improve the visual field
inside a complex non-compliant myomatous uterus.
 |
Figure 2 - Hysteroscopic myomectomy with bipolar
ressectoscope (first surgery). |
Laparoscopic step was then started as planned (Figure 3). After pneumoperitoneum,
no significant fluid volume was visualized inside the
abdominal cavity, confirming massive intravascular absorption of irrigation media. As the
laparoscopic myomectomy was achieved without problem
and patient kept clinically stable, a new uterine pressurization was made in order to finish
the hysteroscopic myomectomy which was
discontinued. This time, another pump was used
(Endoview Hystero-Pump®) limiting both pressure and flow
in order to avoid fluid overload. However,
pulmonary performance (airway pressure and oxygen
saturation) did not allow a safe surgery and once again it had
to be stopped. Surprisingly, 2.000 mL of fluid
were absorbed in less than 10 minutes although
fluid pressure did not exceed the 100 mm Hg limit.
 |
Figure 3 - Laparoscopic myomectomy (first surgery). |
When surgery had finished, the patient was conducted to the intensive care unit (ICU) for
clinical monitoring, where she was appropriately extubated
by the anesthesiologists. Immediate postoperative blood
tests showed metabolic acidosis, high lactate and
chloride levels, and leucocitosis. Chest X-ray showed
bilateral opacity, initially diagnosed by ICU physicians to be a
shock lung secondary to sepsis (Figures 4A and 4B).
A  |
B  |
Figure 4 - Chest X-ray; A: before first surgery; B:
immediately after patient was extubated in intensive care unit (first surgery). |
|
After discussing the case with the anesthesiologists, infectious etiology was
immediately excluded because the cause was obvious: a
non-cardiogenic pulmonary edema secondary to an iatrogenic saline overload in a previously
healthy patient. Although pleural effusion caused
symptoms (Figures 5 and 6), the treatment mainstay was
non-invasive positive pressure ventilation and diuretics.
The discharge from hospital occurred after 1 week
(Figure 7).
 |
Figure 5 - Chest X-ray (lateral decubitus); third day. |
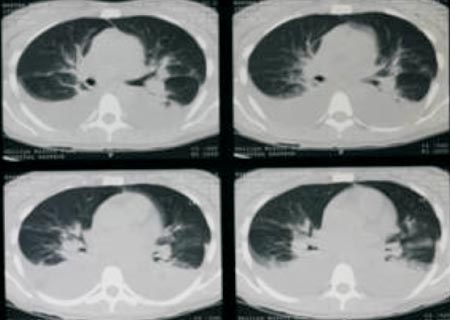 |
Figure 6 - Computerized axial tomography scan showing
pleural effusion; third day. |
 |
Figure 7 - Discharge from hospital after one week (first surgery). |
A second hysteroscopic surgery (Figure 8) was conducted under spinal anesthesia 1 month
after discharge for concluding myomectomy, without complications. However, fluid absorption was
high again: 2.500 mL after only 20 minutes of surgery
using saline in Endoview Hystero-Pump® system.
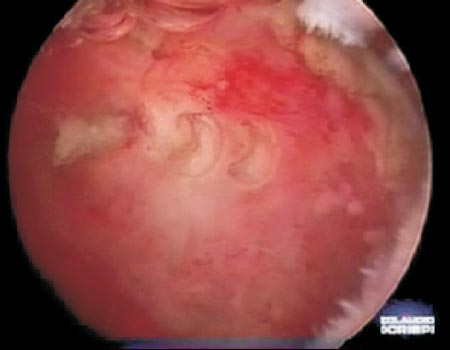 |
Figure 8 - Uterine cavity view at the end of the second
surgery (without fibroids). |
DISCUSSION
Besides transurethral resection of the
prostate, operative hysteroscopy (OH) is an endoscopic
surgery in which undesirable absorption of irrigation fluids is
a major risk factor for
complications1,2,3,4,5. Actually, the excessive intravasation of the fluid used to
distend and irrigate the uterine cavity is the most
dangerous complication during hysteroscopic
myomectomy6. Long surgeries, high intrauterine pressures, and
fibroid resection (myomectomy) favor high distension
media absorption during surgical procedure;
significant intravasation and high risk of fluid overload may
be present as well. Complications such as
cardiovascular collapse and noncardiogenic pulmonary edema
may occur if large volumes of any distension media
are rapidly absorbed7,8,9,10,11. Moreover, fluid
overload becomes quite dangerous when a solution
lacks electrolytes (i.e. sodium) because of the risk
of dilutional hyponatremia and cerebral
edema12,13,14.
Our team considered saline as the safest distension media. However, its safety can not
be overestimated. This case suggests a concomitant uncommon uterine condition which predisposed
this patient to massive absorption and fluid overload.
A multiple myomatous uterus more likely shows low compliance for fluid distention and
high vascularization; these conditions may have a
higher chance of transforming hysteroscopic surgery into
a more complex and risky procedure2,11. We
suggest repeated fluid balance (ex. after each two liters
of irrigation) and a frequent evaluation about the possibility of stopping surgery if a tendency to
high absorption is occurring. Using this strategy,
time becomes not important but the absorbed fluid
volume must be continually monitored.
Actually, there is no rule for defining a maximum fluid input because patients are not
the same. However, pressure must be set as low as possible, particularly if the fluid lacks
sodium12,13,14 (ex. sorbitol, manitol and glycine). If the
distension media is NaCl 0.9% (bipolar system), the
capacity to tolerate fluid absorption will be higher and it
will depend on body mass, age and cardiovascular
status. Of course, hyponatremia will not be problem
with saline12,13,14.
Nowadays, with basis on American College of Obstetricians and
Gynecologists15, our team has adopted a more rigid strategy to prevent fluid
overload allowing maximal time in hysteroscopic
surgery10,11:
A- Begin surgery with fluid pressure of
about 100 mm Hg until uterine distension and panoramic
view are satisfactory; B- Decrease pressure as low
as possible to maintain satisfactory surgical field (Ex.
70-80 mm Hg - maybe less); C- Check fluid
balance after each 2 L of pumped solution: [Absorbed
fluid = pumped - recuperated]; D- Keep yourself
alert for the tendencies in absorption by avoiding
"surprises" considering the sum of absorbed fluid after each
fluid verification (pressure can be changed when necessary);
E- Evaluate the possibility of interrupting the procedure if 1 L were absorbed
(non-electrolytic solution) and administer furosemide 0.5 - 1
mg/Kg; F- End surgery if absorption hits 1.5 L
(non-electrolytic solution) and measure blood-sodium for
follow-up (Attention: fast absorptions are more dangerous
than slow ones!).
Obs. If bleeding becomes expressive and/or if fluid bags are significantly overfilled,
Absorbed fluid can become
negative5,6,16.
CONCLUSION
If fluid intravasation is frequently monitored and the lowest pressures are tried when possible,
time will not be so important. Besides, while surgeon
is sure about the intravasation, general anesthesia
can be as safe as epidural or spinal anesthesia and
there is the added benefit that patient does not need to
be awake during surgery. Surgeon, anesthesiologist
and nurse should be a team.
REFERENCES
1. Julian TM. Hysteroscopic complications. J Low Genit
Tract Dis 2002; 6: 39-47.
2. Sardo ADS, Mazzon I, Bramante S, Bettocchi S, Bifulco
G, Guida M, Nappi C. Hysteroscopic myomectomy: a comprehensive review of surgical techniques. Human
Reprod Update. 2008; 14:101-119; doi:10.1093/humupd/dmm041.
3. Indman PD, Brooks PG, Cooper JM, Loffer FD, Valle
RF, Vancaillie TG. Complications of fluid overload from
resectoscopic surgery. J Am Assoc Gynecol Laparosc 1998; 5: 63-7.
4. Rassweiler J, Teber D, Kuntz R, Hofmann R.
Complications of Transurethral Resection of the Prostate
(TURP)—Incidence, Management, and Prevention. Eur Urol 2006;
50: 969-80.
5. Sutton C. Hysteroscopic surgery. Best Pract Res Clin
Obstet Gynaecol 2006; 20: 105-37.
6. Nezhat CH, Fisher DT, Datta S. Investigation of
often-reported ten percent hysteroscopy fluid overfill: Is
this accurate? J Minim Invasive Gynecol 2007; 14: 489-93.
7. Mushambi MC, Williamson K. Anaesthetic
considerations for hysteroscopy surgery. Best Pract Res Clin
Anaesthesiol 2002; 16: 35-51.
8. Schäfer M, Ungern-Stemberg BSV, Wight E, Schneider
MC. Isotonic fluid absorption during hysteroscopy resulting in
severe hyperchloremic acidosis. Anesthesiology 2005; 103: 203-4.
9. Brandstrup B. Fluid therapy for the surgical patient.
Best Pract Res Clin Anaesthesiol 2006; 20: 265-83.
10. Fonseca MF, Nogueira EA, Gemal AE, Andrade
JLG: Anestesia em videocirurgia: fundamentos para o
cirurgião, Tratado de Videoendoscopia Ginecológica, 2nd edition.
Edited by Claudio Peixoto Crispi. Rio de Janeiro, Atheneu,
2006, pp 75-89.
11. Fonseca MF, Andrade Jr CM, Nogueira EA, Santos
LCS, Crispi CP. Is time monitoring really necessary for
preventing fluid overload in hysteroscopic surgery? A case
report. Presented at: IV International Conference on
Minimally Invasive Gynecologic Surgery - Sobenge; September
27-30, 2006; Rio de Janeiro-RJ; Brazil.
12. Adrogué HJ, Madias NE: Hyponatremia. N Engl J
Med 2000; 342: 1581-89.
13. Fukagawa M, Kiyoshi K, Papadakis MA: Fluid
& electrolyte disorders, Current Medical Diagnosis
& Treatment, 55th edition. Edited by Tierney Jr LM,
McPhee SJ, Papadakis MA. The McGraw-Hill Companies.
2006, pp 865-95.
14. Ananthanarayan C, Paek W, Rolbin SH, Dhanidina
K. Hysteroscopy and anaesthesia: review article. Can J
Anaesth 1996; 43: 56-64.
15. ACOG Technology Assessment in Obstetrics
and Gynecology No.4. Hysteroscopy. American College
of Obstetricians and Gynecologists. Obstet Gynecol 2005;106:439-42.
16. Fonseca MF, Andrade Jr CM, Miranda AP, Santos
LCS, Crispi CP. Intravazamento em cirurgia histeroscópica:
Incertezas no volume infundido. Presented at: VIII
Congresso Brasileiro de Videocirurgia _ SOBRACIL; April
28-May 1st, 2007; Bento Gonçalves-RS; Brazil.
Correspondence address:
Márlon de Freitas Fonseca, M.D., M.Sc., Ph.D.
Serviço de Anestesiologia. Instituto Fernandes Figueira - Fiocruz.
Av. Rui Barbosa, 716
Flamengo - Rio de Janeiro - RJ, Brasil
CEP 22250-020
E-mail: marlon@biof.ufrj.br or marlon@iff.fiocruz.br
Phone: 55 21 3972-6357 (residence); 9631-9500 (mobile)
Fax: 55 21 2553-6730