|
|
Official Journal of the
|
|
|
| Original Article « PDF file » |
|
Laparoscopic Lateral Ovarian Transposition
Francisco Furtado1; William Kondo2
1 Gynecologist at Fertway Human Reproduction Center and Hospital Vita Batel, Curitiba - Paraná; 2 General Surgeon at Fertway Human Reproduction Center and Hospital Vita Batel, Curitiba - Paraná.
ABSTRACT
Introduction: Transposition of the ovaries outside of the pelvis to protect them from pelvic radiation was initially
described in 1958. The procedure is indicated in patients diagnosed with malignancies that require pelvic radiation, but not
removal of the ovaries, as part of their treatment. It can be performed by laparotomy or laparoscopy, depending on
gynecologist's surgical skill. The aim of this article is to describe the technique of lateral ovarian transposition by laparoscopy.
Surgical Technique: The patient is placed in Trendelenburg position, under general anesthesia. Pneumoperitoneum is
insufflated using Veress needle and four abdominal trocars are placed: 10mm at the umbilicus, 10mm at the suprapubic
region, and two 5mm at the anterior superior iliac spine bilaterally. The ovaries are completely separated from the uterus
and fallopian tubes by dividing the utero-ovarian ligament and incising the mesovarium. The peritoneum along the
infundibulo-pelvic ligament can be also incised and the ovaries are transposed laterally to the paracolic gutters and sutured.
Two titanium clips are placed at the ovaries to mark the most cephalad and caudal extent. It allows postoperative
localization of the ovaries to program pelvic radiation. Conclusion: Lateral ovarian transposition can be performed safely and
effectively. Laparoscopic approach has some advantages compared to open surgery, including reduced length of hospital stay,
less postoperative pain, smaller incisions and faster recovery. For these reasons, we advocate laparoscopy as the
gold standard approach for ovarian transposition.
Key words: Laparoscopy, ovarian transposition, cancer, radiation.
Bras. J. Video-Sur, 2008, v. 1, n. 2: 057-060
| Accepted after revision: May, 02, 2008. |
INTRODUCTION
adiation therapy is one of the treatment modalities used in the management of patients with
cancer, notably in cases of Hodgkin's disease,
genitourinary and low intestinal tumors. Depending on the site
and the extent of the disease, radiation can be
administered locally or to a larger
area1,2. It is a highly effective therapy in patients with early stage cancers, but it
may result in the loss of ovarian function and in the
necessity of long-term hormone replacement therapy for
young women3. The role of the gynecologist becomes
very important in these cases as an attempt to
preserve the ovarian function, therefore assuring patient's
quality of life and in some cases possible future fertility.
Transposition of the ovaries out of the field
of irradiation to preserve ovarian function was
initially described in 19584. Since then a number of
techniques have been reported, and they were performed
during staging laparotomy or as a separate
procedure5-11. Among them lateral ovarian transposition (rate
of success until 83%)7, ovarian transposition behind
the uterus, ovaries protection with a lead
shield12, exteriorization of the ovaries under the skin
through an opening in the flank8, and heterotopic
ovarian transplantation9.
Recently surgical techniques progress and minimally invasive techniques development
have allowed laparoscopic lateral ovarian transposition
to be performed effectively by
laparoscopy2, with a shorten hospital stay, earlier mobilization, earlier
return to normal activities and reduced
costs13.
The objective of this manuscript is to describe the laparoscopic ovarian transposition
surgical technique.
SURGICAL TECHNIQUE
The operation was performed under general anesthesia. The patient was placed in
lithotomy Trendelenburg position with both legs protected
by elastic bandages. A Foley catheter was inserted
into the urinary bladder for continuous monitoring of
urine output during the operation.
Pneumoperitoneum was then insufflated with Veress needle and pressure maintained between
12 to 14mmHg. A 10-mm trocar was placed at the umbilicus for the
0o optical, a 10-mm trocar was place at the suprapubic area and two 5-mm trocars
were placed at the anterior superior iliac spine bilaterally.
The procedure began with a thorough examination of the abdominal cavity searching
for eventual metastasis, including the liver and
the diaphragm. The utero-ovarian ligaments were electrocauterized and divided (Figures 1A, 2A
e 2B). The same procedure was performed on the mesovarium. The dissection was continued to
the infundibulopelvic ligament with attention to
leave the vascular pedicle inside the ligament
intact. Ovaries were mobilized to the level of the
anterior-superior iliac spines. In case of
inadequate mobilization, a relaxing incision could be made
on the peritoneum inferior to the ovary. It is not necessary to transect the fallopian tubes
performing this technique which will increase the chances of
a future pregnancy as patient's wish. The ovary
was anchored.
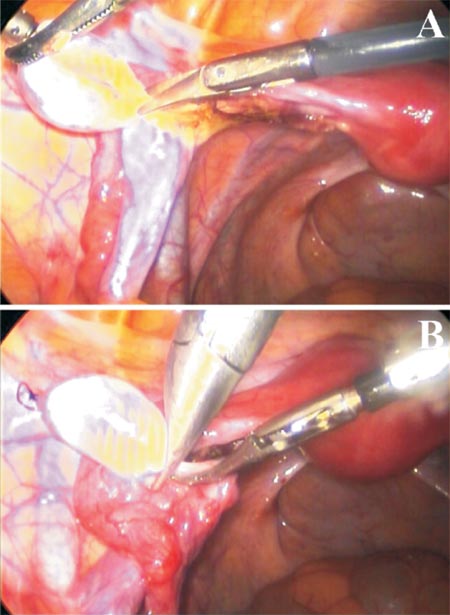 |
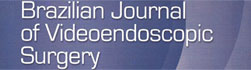
Figure 1 - (A) Left utero-ovarian ligaments section. (B) The
ovary is fixed to the left paracolic gutters and marked by a metal clip. |
To the peritoneum with two sutures of inabsorbable thread (Figures 1B e 2C). The
inferior border of the ovary was marked with a vascular
metal hemoclip bilaterally (Figures 1B e 2D) in order
to be found during radiation.
 |
Figure 2 - (A e B) Right utero-ovarian ligaments section and coagulation. (C) The right ovary is fixed to the right paracolic gutters.
(D) Right ovary marked by a metal clip. |
FOLLOW-UP
Measurement of follicle-stimulating hormone (FSH) is obtained before the surgical procedure. The ovarian function is evaluated by monitoring patient's menstrual cycles and eventual symptoms of ovarian failure. Postoperatively it is important to perform a Doppler ultrasound of the pelvic region to assure the presence of blood flow in the transposed ovaries. Control of the ovarian function is checked by the measurement of FSH 30 days after the surgery and 30 days after completing radiotherapy.
DISCUSSION
The advent of laparoscopy was one of the most important innovations in modern-day surgery
and many procedures that previously required a
laparotomy now could be done by minimally invasive
access2,14. Patients undergoing laparoscopic surgery
have experienced shorter hospitalization, smaller
incisions, less postoperative pain, faster recovery and more
rapid return to radiotherapy without complicating
subsequent therapeutic protocol than patients receiving
the traditional abdominal approach15. This could be
done to ovarian transposition.
Ovarian preservation seems mandatory for premenopausal young patient with
non-hormone-dependent gynecologic cancers or
nongynecologic cancers requiring pelvic
irradiation14,16. The ovaries have been transposed to a variety of sites;
however there has not been a consensus. Usually they are
placed as high or lateral as possible
15,17, but the ovaries can also be transposed medially behind the uterus or
to any distant site1.
Other methods include ovaries protection with a lead
shield12 (it seems less effective than
ovaries lateralization, besides it protects compromised
lymph nodes), exteriorization of the ovaries under the
skin through an opening in the flank(this technique has
been associated to ovarian cyst formation)
8, and heterotopic ovarian transplantation (implantation of the ovary
to the medial face of the arm using vascular
anastomosis)9.
According to Treissman e cols. 18,
ovarian suspension with transection of the ovarian
ligament allows an adequate mobilization of the ovaries. In
some cases an additional relaxing incision on the
peritoneum inferior to the ovary may be needed. This
laparoscopic technique is simple, as dissection of the cecum is
not necessary and the fallopian tubes can be stretched
up to the level of the anterior-superior iliac spines.
Lateral ovarian transposition by laparotomy has been associated with preservation of
ovarian function in 83% of patients after pelvic
irradiation7. Successful preservation of the ovarian
function depends on two factors: the dose of radiation
received by the ovary and the age of the
patient14,19. In the study of Huang and
cols3, eight out of the fourteen patients (57.1%) had ovarian failure after
laparoscopic ovariopexy. Among the patients older the 40 years
of age, 6 out of the 7 patients (85.7%) developed
ovarian failure after the surgery, while among the patients
in age below 39 only 1 out of the 7 patients (14,3%)
had ovarian failure. Thus, ovarian failure happens not
only just because the relevant vessels are disrupted
during the procedure, but also because older ovaries are
more sensitive to chemotherapy and
radiotherapy1,16,19.
Possible complications of ovarian transposition are torsion of the ovarian vascular
pedicle7, ureter injury, intraoperative bleeding, functional ovarian
cyst formation and subsequent recurrence on
transposed ovaries20,21.
In this manuscript we described the laparoscopic lateral ovarian transposition
surgical technique. Besides the benefits above mentioned
of the minimally invasive procedure, laparoscopic
surgery theoretically causes less pelvic adhesion
compared with laparotomy3. As it is a simple and
minimally invasive technique laparoscopy is a gold
standard approach for ovarian transposition.
REFERENCES
1. Bisharah M, Tulandi T. Laparoscopic preservation of
ovarian function: an underused procedure. Am J Obstet
Gynecol 2003;188: 367-70.
2. Tulandi T, Al-Took S. Laparoscopic ovarian
suspension before irradiation. Fertil Steril 1998; 70: 381-3.
3. Huang KG, Lee CL, Tsai CS, Han CM, Hwang LL. A
new approach for laparoscopic ovarian transposition before
pelvic irradiation. Gynecol Oncol 2007; 105: 234-7.
4. McCall ML, Keaty EC, Thompson JD. Conservation
of ovarian tissue in the treatment of carcinoma of the
cervix with radical surgery. Am J Obstet Gynecol 1958; 75:
590-600.
5. Belinson JL, Doherty M, McDay JB. A new technique
for ovarian transposition. Surg Gynecol Obstet 1984; 159:
157-60.
6. Gabriel DA, Bernard SA, Lambert J, Croom RD
3rd. Oophoropexy and the management of Hodgkin's disease.
A reevaluation of the risks and benefits. Arch Surg 1986;
121: 1083-5.
7. Husseinzadeh N, Nahhas WA, Velkley DE, Whitney
CW, Mortel R. The preservation of ovarian function in
young women undergoing pelvic radiation therapy. Gynecol
Oncol 1984; 18: 373-9.
8. Kovacev M. Exteriorization of ovaries under the skin
of young women operated upon for cancer of the cervix. Am
J Obstet Gynecol 1968; 101: 756-9.
9. Leporrier M, von Theobald P, Roffe JL, Muller G. A
new technique to protect ovarian function before pelvic
irradiation. Heterotopic ovarian autotransplantation. Cancer 1987;
60: 2201-4.
10. Nahhas WA, Nisce LZ, D'Angio GJ, Lewis JL Jr.
Lateral ovarian transposition. Ovarian relocation in patients
with Hodgkin's disease. Obstet Gynecol 1971; 38: 785-8.
11. Ray GR, Trueblood HW, Enright LP, Kaplan HS,
Nelsen TS. Oophoropexy: a means of preserving ovarian
function following pelvic megavoltage radiotherapy for
Hodgkin's disease. Radiology 1970; 96: 175-80.
12. Thomas PR, Winstanly D, Peckham MJ, Austin DE,
Murray MA, Jacobs HS. Reproductive and endocrine function
in patients with Hodgkin's disease: effects of
oophoropexy and irradiation. Br J Cancer 1976; 33: 226-31.
13. Visvanathan DK, Cutner AS, Cassoni AM, Gaze M,
Davies MC. A new technique of laparoscopic ovariopexy
before irradiation. Fertil Steril 2003; 79: 1204-6.
14. Clough KB, Goffinet F, Labib A, Renolleau C, Campana
F, de la Rochefordiere A, et al. Laparoscopic unilateral
ovarian transposition prior to irradiation: prospective study of
20 cases. Cancer 1996; 77: 2638-45.
15. Lee CL, Lai YM, Soong YK, Lin TK, Tang SG.
Laparoscopic ovariopexy before irradiation for medulloblastoma.
Hum Reprod 1995; 10: 372-4.
16. Ishii K, Aoki Y, Takakuwa K, Tanaka K. Ovarian
function after radical hysterectomy with ovarian preservation
for cervical cancer. J Reprod Med 2001; 46: 347-52.
17. Classe JM, Mahé M, Moreau P, Rapp MJ,
Maisonneuve H, Lemevel A, et al. Ovarian transposition by
laparoscopy before radiotherapy in the treatment of Hodgkin's
disease. Cancer 1998; 83: 1420-4.
18. Treissman MJ, Miller D, McComb PF. Laparoscopic
lateral ovarian transposition. Fertil Steril 1996; 65: 1229-31.
19. Morice P, Castaigne D, Haie-Meder C, Pautier P, El
Hassan J, Duvillard P, et al. Laparoscopic ovarian transposition
for pelvic malignancies: indications and functional
outcomes. Fertil Steril 1998; 70: 956-60.
20. Morice P, Haie-Meder C, Pautier P, Lhomme C,
Castaigne D. Ovarian metastasis on transposed ovary in
patients treated for squamous cell carcinoma of the uterine
cervix: report of two cases and surgical implications. Gynecol
Oncol 2001; 83: 605-7.
21. Anderson B, LaPolla J, Turner D, Chapman G, Buller
R. Ovarian transposition in cervical cancer. Gynecol Oncol
1993; 49: 206-14.
Correspondence address:
William Kondo
Av. Getúlio Vargas, 3163 ap 21
Curitiba - PR
Telephone: (41) 9222-1065
E-mail: williamkondo@yahoo.com