|
|
Official Journal of the
|
|
|
| Original Article « PDF file » |
|
Veress Needle Insertion in the Left Hypochondrium in Creation of the Pneumoperitoneum: Validation of the Technique, Value of Tests and Importance of Intraperitoneal Pressure and Volume of Gas Injected During Insufflations
João Luiz Moreira Coutinho Azevedo1; Otávio Cansanção Azevedo2; Otávio Monteiro Becker Junior3; Octávio Henrique Mendes Hypólito4; Afonso César Cabral Guedes Machado5; Dalmer Faria Freire6
1 Associate Professor and Chief of the Section of Videosurgery, Division of Operative Technique, Department of Surgery, Federal University of São Paulo, Mentor Professor of Federal University of São Paulo, Ex-invited Professor and PhD at Lyon University, France; 2 Doctor in Science at UNIFESP. Fellow PhD at UNIFESP. Assistent Doctor Gastroenterology Surgical Service at Hospital do Servidor Público of São Paulo State (HSPE); 3 Fellow PhD of Surgery and Experimentation Program of UNIFESP. Superintendent at the Hospital Municipal de Guarulhos, and Surgeon and Coordinator of Medical Internship at Hospital Municipal de São José dos Campos/UNIFESP-SP; 4 Fellow PhD at Surgery and Experimentation Program of UNIFESP. Coordinator of the Internship Program in Anesthesiology at Hospital Municipal de São José dos Campos/UNIFESP; 5 Postgraduate student at the Surgery and Experimentation Program of UNIFESP. Coordinator of the Medical Internship at Hospital Municipal São José dos Campos/UNIFESP, SP. Vice-Professor of the Brazilian College of Surgeons, SP. Member of the Brazilian College of Digestive Surgery, SP; 6 Fellow PhD of the Surgery and Experimentation post-graduation program at UNIFESP. Chief of the Service of Surgical Clinic at Hospital Municipal de Campo Limpo, SP.
ABSTRACT
Objectives: To validate the efficacy of Veress needle insertion into the left hypochondrium, to evaluate the
accuracy of the tests used to check the position of the needle, and to establish parameters for pressure and volume
at different moments of insufflations. Methods: It was compared thirty-two patients who were punctured into
the abdominal midline (ML group), to 30 patients into the left hypochondrium (LH group). Afterwards, 70 patients
were also punctured in the left hypochondrium and, together with those of the LH group, comprised a total of
100 patients of the left hypochondrium (TLH) group. Tests were performed and considered positive when:
organic material was aspirated in the aspiration test (AT) ; only a small amount of pressure was applied to inject the
liquid in the injection test (IT); the injected liquid was not recovered in the recovery test (RT) ; drops drained quickly in
the hanging drop test (HDT); pressure levels were 8 mmHg or lower in the initial intraperitoneal pressure test
(IIPT). Sensitivity (S), specificity (SP), positive predictive value (PPV) and negative predictive value (NPV) were
established for each test. Volume and pressure were recorded at every 20 seconds, until intraperitoneal pressure
reached 12 mmHg. Pressure and volume values were correlated with predetermined moments of insufflations.
Results: two failed attempts at creating pneumoperitoneum were observed in the ML group and three in the LH group.
In the TLH group, ten failed attempts were observed. For the AT, S and PPV could not be determined, SP = 100%
and NPV = 100%. For the IT, S = 100%, SP = 0%, PPV = 90%, and NPV could not be determined. For the RT and
SDT, S = 100%, SP = 50%, PPV = 94.7% and NPV = 100%. For the IIPT, S, SP, PPV and NPV were 100%. Pressure
and volume showed a strongly positive correlation with predetermined moments of insufflations (coefficient
of explanation of 0.8011and 0.9604, respectively). Conclusions: Punctures in the left hypochondrium are
effective. The tests assessed can guide surgeons. Values of pressure and volume at predetermined moments
of insufflations can be predicted.
Key words: Laparoscopy, adverse effects. Surgical procedures, operative. Pneumoperitoneum, artificial.
Punctures, adverse effects. Punctures, methods.
Bras. J. Video-Sur, 2008, v. 1, n. 1: 020-028
| Accepted after revision: January, 11, 2008. |
INTRODUCTION
he access to the peritoneal cavity is the most
critical step of laparoscopy, in which the
majority of severe transoperative complications
occur17. Even though there is no consensus with regard to the
best method of accessing the peritoneal cavity for
creation of the pneumoperitoneum17; puncture with
Veress needle is the most frequently used
technique16. A study of 155.987 laparoscopic procedures was
performed in which the Veress needle was used in 81%.
However, great vessels and abdominal viscera injuries may occur when Veress needle is
blindly inserted into the abdomen before the
insufflation1. In spite of being rare (prevalence of
0,05%)24, major vascular injury caused by the Veress needle or by
the primary trocar is the most frequent cause of death
in laparoscopic procedures(15%)1. Additionally, it
is difficult to diagnose this complication because of
the retroperitoneal vessels position22. Under
these conditions bleeding seldom occurs in the
peritoneum and the retroperitoneal hematoma is not always visible.
The traditional site of the insertion of the Veress needle is the abdominal midline near
the umbilicus and puncture is considered a risk due to
the close proximity of the anterior abdominal wall to
the retroperitoneal vascular structures, inasmuch in
thin people, this distance can be less than 2
cm1. The abdominal aorta, inferior vena cava and iliac vessels
are particularly prone to injuries during the insertion
of the Veress needle close to the
umbilicus13. Due to the great vessels localization, it is assumed that the risk
of iatrogenic injury is minimized when the punctures
are done away from the midline20,23.
In addition to that, patients with previous abdominal surgery are at increased risk for
visceral injury caused by the Veress needle due to
peritoneal adhesions, which typically occur at the level of
the scar where the surgical incision of the anterior
parietal peritoneum is made20. Autopsy studies have
found adhesions in 74% to 95% of patients with
previous abdominal surgery1. Midline incisions present a
high risk for adhesions in the umbilical region.
Nonetheless, even abdominal incisions performed in a region
not close to the umbilicus may be a cause of adhesion
in the periumbilical region1, as it was reported
by Audebert and Gomel(2000) 4 who showed
the frequency of peritoneal adhesions in the
umbilical region and estimated possible risk for visceral
lesions in case of insertion of instruments in 814
patients examined through minilaparoscopy of the
left hypochondrium. Prevalence of adhesions at the
umbilical region and the arbitrated possible risk in
patients without previous abdominal surgery was of 0,68%
and 0,42% respectively; 1,6% and 0,8% in previous laparoscopy; 19,8% and 6,87% in suprapubic
horizontal laparotomy; and 51,7% and 31,46% in
patients submitted to midline laparotomy.
On the other hand, puncture of the left hypochodrium have been reported as a safe
procedure without a major iatrogenic
risk20,23. The greater omentum, the stomach and the transverse colon
are the closest anatomic structures to the anterior
abdominal wall5. Small autolimited hematomas and
tissular bullous emphysema which are promptly absorbed
are the results of the accidental insertion of the
needle followed by the insufflation of the greater
omentum. The accidental perforation of the stomach by
the Veress needle does not mean that its contents
will necessarily leak considering the triple muscular
layer of the stomach wall which usually obstructs
the puncture hole. Additionally, gas extravasations
through the orogastric tube contribute to accidental
perforation suspicion. In order to minimize the risk for lesions
in the colon, before the puncture patients are placed
in 20 degrees inclined position to allow the movement
of the segments of the large bowel (transverse colon
and descending colon) to the inferior part of the
abdomen, and therefore avoiding eventual punctures.
Punctures caused by the Veress needle in the colon or
stomach are easily diagnosed in the initial examination of
the peritoneal cavity and puncture injuries may be
sutured through laparoscopy.
Besides supporting argument of the left hypochondrium puncture is that peritoneal
adhesions (a risk factor for iatrogenic lesions) seldom occur
in the abdominal wall, because respiratory movement
of the diaphragm constantly holds the left
hypochondrium motile structures, thus making adhesions difficult
to happen in the anterior abdominal wall site. For
these reasons, left hypochondrium puncture is the
best choice for some surgeons in patients with
previous laparotomy23.
There are surgeons that perform bariatric surgeries, and prefer the left hychondrium
puncture for creation of
pneumoperitoneum29. This preference is due to the fact that in obese patients midline
puncture is a hazardous procedure considering the amount
of intra-abdominal fat tissue which may obstruct the
tip of the needle making difficult the insufflation
control. In obese patients there is an increased risk of
lesions due to the fact that the position of the belly button
in the abdomen13 is higher than in non-obese
patients causing a superposition of the puncture site at
the umbilicus level to the intra-abdominal prominence
of retroperitoneal great vessels.
It is important to notice that injuries caused by blind insertion of the Veress needle into the
abdominal midline not only occur in the hands of inexperienced
surgeons. Schafer et al.28 (2001)
verified that among 26 injuries analyzed only 4 of them
(15%) were caused by inexperienced surgeons
(surgeons who had performed fewer than 50
laparoscopic procedures); however 22 injuries (85%) had
been caused by experienced surgeons (those who had performed between 51 and 100
laparoscopic procedures) or very experienced surgeons (over
100 laparoscopic procedures performed). In conclusion,
it is important to emphasize that recently in a
systematic literature review2 it was established that all
the retroperitoneal great vessels injuries by Veress
needle were caused by midline puncture performed near
to the umbilicus. There were any injuries caused
by puncture in the left hypochondrium.
However, in spite of the advantages of the Veress needle insertion in the left hypochondrium
in respect to the midline puncture safety there is not
in the literature a study comparing the efficacy
between the two approaches. Therefore, further
researches are necessary in order to demonstrate
the effectiveness of the left hypochondrium
puncture towards gold standard procedure (midline puncture).
As well as the accuracy of the tests described in
textbooks9,15,18 regarding to intraperitoneal
correct position of the tip of the needle after puncture
and before insufflation was not properly determined.
On the other hand, objective data for surgeons during insufflation are that they should
consider intraperitoneal pressure levels and the amount of
volume injected each time of the insufflation and
values may be associated or not to the tip of the Veress
needle inside the intraperitoneal cavity. These
researches have not been done in humans, but in
pigs3.
The objectives of this study are: to evaluate the efficacy of Veress needle insertion into the
left hypochondrium _ thus validating this technique,
to investigate the accuracy of the tests used to
check the position of the Veress needle in the peritoneal
cavity before the insufflation, and to establish
intraperitoneal pressure and the injected volume values at
different moments of insufflations which will enable to
indicate the correct position of the tip of the needle.
METHODS
This prospective and randomized clinical study was approved by the Research Ethics Committee
of the Health Care Institute for the State Civil
Servant (no45/03), and by the Research Ethics Committee
of the Federal University of São Paulo
(no1405/03).
A total of 132 non-obese - Body Mass Index (BMI) less than 30 _without previous peritonitis
or peritoneal cavity surgery adult patients were
included in this study. These patients were submitted
to laparoscopic procedures at the Gastroenterology Surgical Service at Hospital do Servidor Público
of São Paulo State. A Veress needle was inserted
into the abdominal wall of the patients in order to
create an artificial peritoneum through carbon
dioxide insufflation.
The first 62 patients were randomly distributed in LH group (n=30) _ left hypochondrium
punctured, and ML group (n=32), midline abdominal puncture
at umbilicus level. The two groups were equally distributed regarding to age, sex, BMI, height,
weight and clinical condition (p> 0,05) what have
motivated the programmed surgical intervention.
Afterwards, seventy consecutively scheduled patients were studied whom were punctured in
the left hypochondrium and with the group LH
(n=30) comprised the TLH _ total left hypochondrium
group (n=100).
The mean age in the TLH group was 53,7 years (± 13,1), ranging from 27 to 77 years old.
There were 58 women and 42 men in the study. The
mean body mass index (BMI) was 25,6 (± 2,4) _
ranging from 20,6 to 29,7. There were 80
cholecystectomies, 9 Nissen fundoplication to treat
gastroesophageal reflux disease and 11 inguinal hernioplasties.
Thirty minutes before the anesthesia 0,1mg/kg midazolan was administered. Induction
of anesthesia was obtained with propofol 2mg/kg
and 0,5mcg/kg of phentanyl, and for curatization
0,5mg/kg of atracurium was used. Patients were
submitted to general anesthesia with orotracheal intubation
and controlled mechanical ventilation. An orogastric
probe was inserted thus the stomach contents was aspirated.
Patients placed in 20 degrees inclined position were puncture by a Veress
needle in the umbilicus (ML group) or in the left hypochondrium (LH and
TLH groups). In the LH and TLH groups the Veress
needle was perpendicularly inserted at the costal margin,
8 cm from the midline (figure 1). Four tests
(aspiration, injection, recovery and hanging drop test)
were performed to test the intraperitoneal needle
positioning after puncture and before insufflation. These
tests were considered positive: in the aspiration test
when no organic material was aspirated; in the injection
test when moderate resistance in the syringe was necessary to liquid flow; in the recovery test
when the liquid injected was not recovered and in the
hanging drop test when quick drop flow was
observed. Following an initial intraperitoneal pressure test
(IIPT) was performed with insufflator calibrated at
1,2L/min flow and maximum intraperitoneal pressure
at 12mmHg, and the test was considered positive
when equal or less 8mmHg in the first ten seconds.
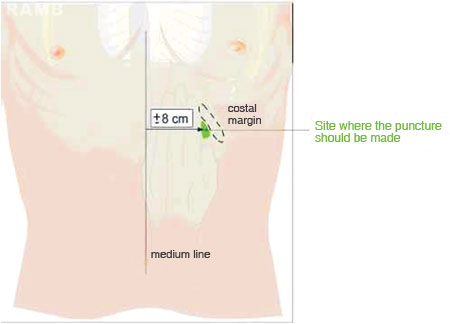 |
Figure 1 - Schematic illustration of puncture in the
left hypochondrium. |
In case of negative and evidence of IIPT preventing the creation of artificial
pneumoperitoneum the whole procedure was considered a failure and
the Veress needle removed from the abdominal wall.
The procedure was then started over again. With
positive IIPT, insufflation of carbon dioxide follows
until pressure reached 12mmHg, thus the whole
procedure was considered a success after the effective
creation of artificial pneumoperitoneum was visually
confirmed through the insertion of a laparoscope inside
the peritoneal cavity. Failed attempts to place the tip
of the Veress needle in the peritoneal cavity were recorded.
Considering all positive tests, insufflation of carbon dioxide proceeded, and variation of
intra-abdominal pressure (IP) and the amount of injected
volume (IV) were computed from zero and in each 20 seconds until maximum programmed IP
(12mmHg) was reached at that moment the duration of
insufflation was reached and registered insufflation time
duration, results were compared between LH and ML groups.
In the TLH group the results were considered to obtain the sensibility (S) and the specificity (Sp)
of each test that was evaluated as well as the
positive predictive values (PPV) and the negative
predictive values (NPV). From the independent
variables (predetermined moments of insufflation _ at
20 seconds intervals), it was also investigated
the possibility to estimate dependent variables value
(intra-peritoneal pressure and amount of injected
volume). Polynomial regression models of first, second and
third degrees were applied and the best adjustment
was determined through residual analysis and
coefficient of determination (R2). Intervals of 95%
confidence level were considered to each model
coefficient estimated. Qualitative variables were represented
by absolute and relative frequencies, and
quantitative variables were represented by mean,
standard deviation, and minimum and maximum
values. Student's t-test and Chi Square test were used
to evaluate the homogeneity among the studied
groups. The significance level considered was 0,05
(á=5%). The equivalence among the studied groups with
respect to intraoperative and postoperative parameters
was determined by confidence intervals (CI
95%) that are shown to each parameter evaluated in each
group. Intervals of 95% confidence level for means
and proportions were considered by standard formulas
for estimators with normal distribution.
Polynomial regression models were applied in order to
evaluate the distribution of intra-abdominal pressure and
injected volume in the peritoneal cavity parameters
regarding to time. The discrepancies (residual) between
the values observed at each time and the ones
adjusted by the model were studied in order to verify data
sets adequacy. Quantities that could not be explained
by the regression equation are the eventual
discrepancies, as for the effect of the omission of external
variables into the model or for the natural variability
among individuals. It was investigated through this
analysis an eventual existence of extreme outliers capable
to altering the estimated curves. It was also tested
the adequacy of the models adjustment comparing to
the previous hypothesis formulated in the adopted
model. In the positive correlations, it was used the
equation to estimate the IP and the IV which was
subtracted from the regression curves in the first, second,
third and fourth minutes of the duration of the
insufflation, in order to establish trustworthy parameters to
the dependent variables estimated values (pressure
and volume) settled at different moments
(independent variables).
RESULTS
Complications were not observed in the punctures performed during the research. The
number of failed attempts to positioning the tip of the
Veress needle correctly in the peritoneum was similar in
the LM and HE groups. Regarding the require time
to conclude the pneumoperitoneum(12mmHg) there was not significant statistical differences between the
two groups. It was not observed variation between
groups with regard to flow and the amount of volume
injected during each moment of insufflation values
of intraperitoneal pressure.
In the total left hypochondrium(TLH) group the maximum number of attempts to create
the pneumoperitonum in each patient was two.
Insufflation did not occur in undesired site. Among ten
failed attempts half of them were identified either by
the Recovery test (RT) or by the hanging drop test
(HDT) and by the initial intraperitoneal pressure test
(IIPT), and the other half was exclusively detected by
the IIPT. Injury absence was correctly detected by
the aspiration test. Resistance test was not able to
detect any of the 10 failed attempts, and recovery test
and hanging drop test was not able to detect 5 out of
10 failed punctures that afterwards were detected by
the IIPT. In the AT, Sensitivity (S) and Positive
Predictive Value (PPV) were not applied, Specificity (Sp)
=100%, and Negative Predictive Value (NPV) = 100%.
In the resistance test, S=100%, Sp=0%, PPV= 90%
and NPV did not occur. In the recovery test and in
the hanging drop test, S=100%, Sp=50%, PPV-94,7%
and NPV=100%. In the initial intraperitoneal pressure
test, S, Sp, PPV and NPV=100%. There was strong positive correlation of time of insufflations
(coefficient of determination 0,8011 and 0,9604) and with
pressure and volume. IP and IV estimation in certain
moments of insufflation is expressed in the Table 1.
 |
DISCUSSION
The creation of pneumoperitoneum by Veress needle insertion in the left
hypochondrium23 is an easy, quick and effective
technique6. The primary trocar may be safely and efficiently inserted after
the peritoneal cavity insufflation, and while the intraperitoneal pressure is at an adequate level
to maintain the intra-abdominal structures distant
from the anterior abdomen wall mainly from the retroperitoneal great vessels suppressing
gas extravasations during surgery. After creation
of pneumoperitoneum through peritoneotomy and insertion of Hasson's
trocar12 extravasations frequently occur. This is very important especially
in obese patients29.
The sites of Veress needle puncture described are the midline of the anterior wall at umbilicus
level (considered as standard site
1,10,19), left subcostal
margin10,23 at the 9th left intercostal
space8, a midpoint in the midline between the xiphoid appendix and
the umbilicus14, and a point identical to
McBurney's point at the left iliac
fossa10. There are also reports of transvaginal access to peritoneal cavity through
uterine fundus transfixation with the needle inserted into
the cervical canal (transfundal technique)
26.
The existence of comparatives studies with alternatives techniques depicted concern with
regard the blind insertion safety of the Veress needle into
the midline.
In a randomized study, Santala e col.
26 compared the conventional method of
midline periumbilical puncture to the transfundal
technique; bleeding, infection or injuries of the pelvic organs
did not occur. However, the transfundal technique is
not indicated to patients with previous
pelvic inflammatory disease and to the ones with possible pelvic
peritoneal adhesions or infertility diagnoses.
Moreover, this procedure possible increases the risk of endometriosis and adenomyosis besides
it is exclusive of female patients. It is also a concern
to establish pneumoperitoneum in an injured organ.
Ostrzensky25 (1999) accomplished a prospective, randomized and blinded study in
200 patients in which it was compared the
conventional method of slightly oblique midline
periumbilical puncture caudad to a technique in which the
Veress needle was inserted forming a very sharp angle
with anterior abdominal wall that was almost in
parallel. The study did not report any differences
between the two techniques effectiveness, thus the
author emphasized the advantages of the
alternative technique in order to prevent injuries to
the retroperitoneal great vessels.
Palmer8 described the Veress needle
insertion into the left hypochondrium 3cm below the
costal margin in the mid-clavicular line. Schwartz et
col.29 (2003) established pneumoperitoneum in 600
patients with morbid obesity by inserting the Veress
needle into the left hypochondrium. There was a
puncture injury in the muscular layer of the transverse
colon which was sutured by laparoscopy. There was
not perforation of any other hollow viscera,
abnormal bleeding of the abdominal or visceral wall, nor
even hepatic or splenic injury. Rothagi et
col. 29 (2003) performed 344 punctures into the left
hypochondrium occurring only two failed attempts. The
only complication was a greater omentum hematoma, which was treated by expectant management.
The authors conclude that puncture into the left hychondrium is effective for
establishing pneumoperitoneum.
In the current research the puncture into the left hypochondrium described by
Palmer20 was modified, and it was established a point to the
insertion of the needle 8cm from the abdominal midline in
order to avoid the risk for injuries in the superior
epigastric vessels6.
Additionally, in this research the instrument was inserted at the inferior costal margin in order
to take advantage of its fixation to the parietal
peritoneum due to the cranial shift of the site of the needle
insertion from the Palmer's point.
Considering that some surgeons usually perform abdominal midline puncture, they argue
that the left hypochondrium technique is more
difficult, therefore several attempts are necessary
to accomplish it. However, this research depicted
that comparing both techniques performed by experienced surgeons it was statistically
equivalent regarding either the amount of time to reach
pre-established intraperitoneal pressures or the
number of successful or unsuccessful attempts to
create pneumoperitoneum. Moreover, punctures were equivalent in both sites with regard to the
needle positioning tests positive results, and to
the progression of values of intraperitoneal pressure
and injected volume. As the needle is placed into different sites of the abdomen (umbilicus region
or left hypochondrium) there could have been discrepancies in regard to the evaluated
parameters due to the abdomen anatomical topography
which it did not occur, thus both techniques
effectiveness were equivalent.
It should also be considered that in the left hychondriun puncture the Veress needle route is at
a distance from the retroperitoneal great vessels
and the superior epigastric vessels6, therefore
possible iatrogenic injury is unlikely to occur with
puncture approach. Besides neither the small bowel lie
beneath the site where the left hypochondrium puncture
is performed, nor the normal-sized spleen or liver are
in the Veress needle route. On the other hand, the stomach, the omenta and the colon are subjacent
to the punctures site and they may be incidentally
injured. Nevertheless, they are not considered major
injuries and they are easily repaired17.
As opposed to what occur in the umbilical region adhesions in the left hypochondrium are
very rare; however, they may be observed in patients
with previous splenectomy or colectomy who need mobilization of the splenic flexure of the
colon. Puncture into the left hypochondrium should not
be performed in these patients.
Regarding the approach performed to create pneumoperitoneum with the Veress needle
insertion, there is not an adequate evaluation concerning
the accuracy of the tests performed to check the
position of the tip of the needle in the peritoneum.
Besides, there are studies in experimental animals but not
in humans3.
In this research the Resistance Test (RT), the Recovery Test(ReT), the Hanging Drop
Test(HDT) and Initial Intraperitoneal Pressure Test(IIPT)
were performed to check an appropriate position (tip of
the needle into the peritoneal cavity) which was
considered positive when through some observed evidences it
was assumed that needle was in the correct position.
When the tip of the needle was not in the peritoneal
cavity these tests were considered negative.
On the other hand, Aspiration Test (AT) was performed to diagnose iatrogenic injuries at the
onset of the puncture procedure, that is, AT was
considered positive when the tip of the needle was inside
the parenchymatous organ, the hollow viscus or the
blood vessel which could be confirmed through fluids
or organic tissues aspiration. The aspiration test has
peculiar characteristics as it is performed to detect
the presence or absence of iatrogenic injuries and not
to check the correct position of the tip of the needle.
In order to grant a better credibility and accuracy to our conclusions and to provide a
better evaluation of the tests, statistical and
mathematical criteria were applied to our results. In order to
detect the intraperitoneal position of the tip of the
Veress needle, the ideal test is considered when
positive indicates without a doubt exactly the tip of the
needle inside the peritoneal cavity and when negative
assures that it is not in the site. Therefore, all the tests
were analyzed according to their sensibility (the ability
to detect true positives), specificity (the ability to
detect true negatives), positive predictive value
(the probability of the correct position of needle
among the positive results obtained) and negative
predictive value (the probability of incorrect position of the
needle among the negative results obtained).
Regarding ResT, RecT, SDT, IIPT, true positives were confirmed by inserting a
laparoscope after pneumoperitoneum had been established
which allowed the tip of the needle inside the peritoneal
cavity to be visualized, while true negatives were
confirmed either by the impossibility of creating pneumoperitoneum or by insufflation into an
inadequate site.
As in this research there was not iatrogenic injuries the AT presented excellent specificity
and NPV (100%); therefore, sensibility and PPV
were not able to be calculated. In order to have an
accurate evaluation of the aspiration a larger sample with
the presence of iatrogenic injuries in this study would
be necessary.
The ResT was not able to detect the incorrect position of the tip of the needle (Sp=0), due to
the subjectivity of the test which depends on the ability
of whom perform it. On the other hand it correctly detected when the tip of the needle is into the
peritoneal cavity with 100% of sensibility. When the test
was positive there was 90% (PPV) probability of
the correct position of the tip of the needle. As there
was not a negative test it was not possible to calculate
the probability of the test being correct (NPV).
Either the RecT or the HDT accurately determined the correct position of the tip of needle
in 100% of the cases (S). The correct position of the
tip of the needle in 94,7% (PPV) of the cases were confirmed by the positivity of the test. These
tests were only able to detect 50% (Sp) of the cases
with regard to the wrong positioning of the needle.
When tests were negatives there was 100% (NPV) probability for the tip of the needle to be placed
outside the abdominal cavity.
The IIPT which is the most reliable tests among the ones studied accurately detect either
the wrong or the correct position of the needle
(100% sensibility, specificity, positive and negative
predictive values).
During the creation of the pneumoperitoneum pre-determined moments of the insufflation
were correlated to the intra-abdominal pressure and to
the injected volume in order to establish
paradigms regarding the dependent variables estimated
values (IP and IV), in relation to the independent
variable (considered insufflation moment), in order to
give mathematical relationship through an equation
capable to interconnect the variables.
Correlation coefficient is a pure number used to classify the correlation in perfect (=1), strong
(>0,75 and < 1), medium (> 0,5 and < 0,75), weak (< 0,5)
and null (= 0)29. In this research either the IP or the
IV depicted a strong correlation.
The insufflators aim to reach a preset intraperitoneal pressure. It is also set a maximum
limit to the insufflation flow. When the insufflation
begins the equipment measure the abdominal pressure
through the eye of the needle, and if the actual pressure is
less than the preset pressure it will allow gas flow. In
this research the flow rate (1,2L/min) was adequate
to the creation of pneumoperitoneum; therefore minimizing harmful hyperreflexia of
the parasympathetic nervous system and providing
exact values to the expected volume in liter per second
(0,2L/s). In order to maintain the desirable
intraperitoneal pressure the flow decreases, when the actual
pressure is close to the preset pressure.
Intraperitoneal pressure or CO2 injected
volume evolution during the creation of pneumoperitoneum have not been described in
the literature.
In this study the intraperitoneal pressure and the injected volume allow the researcher to
anticipate their values during crucial moments of the
insufflation. Therefore, the surgeon could easily monitor
the creation of the pneumoperitoneum and check
whether the intraperitoneal pressure and the injected
volume are accordingly to the estimated values.
If values were not as the estimated, it is necessary to verify if the tip of the needle
is inadvertently outside the peritoneal cavity. The
muscle tension of the abdominal wall (insufficient
anesthetic muscle relaxation) should also be considered a
factor. Besides, the tip of the needle may be obstructed
by abdominal structures, usually the greater omentum.
CONCLUSIONS
In conclusion the Veress needle insertion in the left hypochondrium for creation
of pneumoperitoneum is a safe and effective
procedure; in addition to that the 5 tests are adequate to guide
the surgeon towards the correct positioning of the tip
of the Veress needle, moreover the intraperitoneal pressure and injected volume variables are
efficient parameters at certain moments of insufflation in
order to confirm the correct intraperitoneal site of
the instrument tip.
For this reason, the left hypochondrium puncture technique should be suggested as the
method of choice for creation of pneumoperitoneum,
instead of the traditional abdominal midline puncture at
the level of the umbilicus. It is also recommend
the procedure protocol described in this study to be
adopted by surgeons. Extensive and accurate literature
review clearly reveals the existence of fatal wounds
caused by retroperitoneal great vessels and hollow
viscera injuries produced by the Veress needle insertion in
the abdominal midline, consequently all the
laparoscopic surgeons, mainly the new ones should adopt
the described protocol of this study.
REFERENCES
1. Anaise.D, editor. Vascular and bowel injuries during
laparoscopy [monography of the Internet]. Available from:
http://www.danaise.com/vascular_and_bowel_injuries_duri.htm
2. Azevedo JLMC, Almeida CES, Moreira CH, Azevedo
DC, Becker Junior OM, Ferreira DS. Lesões causadas pela
agulha de Veress durante a criação do pneumoperitônio: revisão
sistemática da literatura. Rev Assoc Med Bras. 2008 (prelo
e online) - http://www.cirurgiaonline.med.br/videocirurgia.htm
3. Azevedo JL, Guindalini RS, Sorbello AA et al. Evaluation
of the positioning of the tip of the Veress needle during
creation of closed pneumoperitoneum in pigs. Acta Cir
Bras. 2006;21:26-30.
4. Audebert AJ, Gomel V. Role of microlaparoscopy in
the diagnosis of peritoneal and visceral adhesions and in
the prevention of bowel injury associated whith blind
trocar insertion. Fertil Steril. 2000;72:631-5.
5. Baba RB, Iriya K. Anatomia cirúrgica do estômago
(incluindo junção esofafogástrica) e duodeno. In:
Gama-Rodrigues JJ, Grande JCD, Martinez JC, editors. Tratado de
clínica cirúrgica do sistema digestório. São Paulo: Editora
Atheneu; 2004. p. 39-48.
6. Balzer KM, Witte H, Recknagel S, Kozianka J, Waleczek
H. Anatomic guidelines for the prevention of abdominal
wall hematoma induced by trocar placement. Surg Radiol
Anat. 1999;21:87-9.
7. Catarci M, Carlini M, Gentileschi P, Santoro E. Major
and minor injuries during the creation of
pneumoperitoneum. Surg Endosc. 2001;15:566-9.
8. Childers JM, Brzechffa PR, Surwit EA. Laparoscopy
using the left upper quadrant as the primary trocar site
Gynecol Oncol. 1993;59:221-7.
9. Coptcoat MJ, Coptcoat AD. General
Laparoscopic Techniques. In: Coptcoat MJ, Coptcoat AD,
editores. Laparoscopy in Urology. London: Blakwell
Scientific Publication; 1994. p. 28-30.
10. Guimarães P. Pneumoperitônio, punções e trocartes.
In: Donadio N, Albuquerque Neto LC. Eds. Consenso
Brasileiro em videoendoscopia ginecológica. São Paulo, Artes
Médicas, 2001. p27-32.
11. Guyatt G, Walter S, Shannon H, Cook D, Jaeschke R,
Heddle N. Basic statistics for clinicians: 4. correlation and
regression. Can Med Assoc J. 1995;152:497-504.
12. Hasson HM. A modifield instrument and method
for laparoscopy. Am J Obstet Gynecol. 1971;13:886-7.
13. Hurd WW, Bude RO, DeLancey JOL, Pearl ML.
The relationship of the umbilicus to the aortic
bifurcation: implications for laparoscopic technique. Obstet
Gynecol. 1992;80:48-51
14. Lee C, Huang K, Jain S, Wang C, Yen C, Soong Y. A
new portal for gynecologic laparoscopy. J Am Assoc
Gynecol Laparosc. 2005;8:147-50
15. Meinero M, Melotti G, Rustichelli G. Entrenamiento y
técnicas básicas. In: Meineiro M, Melotti G, Mouret
Ph, editores. Cirurgía laparoscópica. Madrid: Editorial
Médica Panamericana; 1996. p. 16-27.
16. Molloy D, Kaloo PD, Cooper M, Nguyen TV.
Laparoscopic entry: a literature review and analysis of techniques
and complications of primary port entry. Aust N Z J
Obstet Gynaecol. 2002;42:246-53
17. Mouret Ph. Cirurgia laparoscópica: una evolución de la
filosofia quirúrgica? In: Mineiro M, Melotti G, Mouret
Ph editors. Cirurgía laparoscópica. Madrid. Panamericana,
1996. p.1-12.
18. Nathanson LK. Instrumentos y técnicas operatórias
básicas para cirurgía laparoscópica. In: Cuschieri A, Berci
G, editores. Cirurgía Biliar Laparoscópica. London:
Blakwell Scientific Publication; 1991. p. 18-19.
19. Neudecker J, Sauerland S, Neugebauer E, Bergamaschi
R, Bonjer HJ, Cuschieri A, Fuchs K-H, Jacobi Ch, Jansen
FW, Koivusalo A-M, Lacy A, McMahon MJ, Millat B,
Schwenk W. The European Association for Endoscopic Surgery
clinical practice guideline on the pneumoperitoneum for
laparoscopic surgery. Surg Endosc. 2002;16:1121-43.
20. Palmer R. Safety in laparoscopy. J Reprod Med.
1974;13:1-5.
21. Peterson HB, Greenspan JR, Ory HW. Death
following puncture of the aorta during laparoscopy sterilization.
Obstet Gynecol. 1982;59:133-4.
22. Pirró N, Ciampi D, Champsaur P et al. The
anatomical relationship of the iliocava junction to the lumbosacral
spine and the aortic bifurcation. Surg Radiol Anat. 2005;27:137-41
23. Rohatgi A, Widdison AL. Left subcostal closed (Veress
needle) approach is a safe method for creating a
pneumoperitoneum. J Laparoendosc Adv Surg Tech. 2004;14:278-80.
24. Roviaro GC, Varoli F, Saguatti L, Vergani C, Maciocco
M, Scarduelli A. Major vascular injuries in laparoscopic
surgery. Surg Endosc. 2002;16:1192-6.
25. Ostrzenski A. Randomized, prospective, singleblind trial
of a new parallel technique of Veress pneumoperitoneum
needle insertion versus the conventional closed method. Fertil
Steril. 1999;71:578-81.
26. Santala M, Jarvela I, Kauppila A. Transfundal insertion of
a Veress needle in laparoscopy of obese subjects: a
pratical alternative. Hum Reprod. 1999;14:2277-8.
27. Santor J, Ballagi F, Nagy A, Rákóczi I. A
needle-puncture that helped to change the world of surgery. Surg
Endosc. 2000;14:201-2.
28. Schafer M, Lauper M, Krahenbuhl. Trocar and Veress
needle injuries during laparoscopy. Surg Endosc. 2001;15:275-80.
29. Schwartz ML, Drew RL, Andersen JN. Induction
of pneumoperitoneum in morbidly obese patients. Obes
Surg. 2003;13:601-4.
30. Veres J. Neues Instument zur Ausfuhrung von
Brust-oder Bauchpunktionen und Pneumothoraxbehandlung.
Dtsch Med Wochenshr. 1938;41:1480-1.
Correspondence address:
Prof. Dr. João Luiz Moreira Coutinho Azevedo
Universidade Federal de São Paulo. Prédio da Cirurgia
Experimental Rua Botucatu, 740. Vila Clementino
CEP: 04023-900
São Paulo, SP, Brazil.
Telfax: (xx11) 5576-2472.
Email: jozevedo.dcir@epm.br