|
|
Official Journal of the
|
|
|
| Original Article « PDF file » |
|
New Minimally Invasive Surgical Approaches: Transvaginal and Transumbilical
Anibal Wood Branco1; Alcides José Branco Filho2; Rafael William Noda3; Marco Aurélio de George4; Affonso Henrique Leão Alves de Camargo5; William Kondo6
1 Urologist of CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná; 2 General Surgeon of CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná; 3 General Surgeon e Endoscopist of CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná; 4 General Surgeon of CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná; 5 Urologist of CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná; 6 General Surgeon do CEVIP (Advanced Center of Videolaparoscopy of Paraná), Curitiba - Paraná.
ABSTRACT
Objectives: Since the advent of laparoscopy, surgical techniques have been changing in an attempt to reduce
patient's morbidity, thus less invasive procedures have been used. The aim of this manuscript is to report our experience
in regard to two new minimally invasive surgeries approaches, i.e., the transumbilical laparoscopic surgery (TLS)
and the natural orifices transluminal endoscopic surgery (NOTES). Patients and Methods: Three periumbilical
trocars have been used to perform transumbilical laparoscopic surgery. At completion of the procedure, all three port
incisions were united and the specimen was retrieved from the abdominal cavity. NOTES was performed through
transvaginal access. After opening the vaginal mucosa in the posterior cul-de-sac, a double-channel flexible endoscope
was inserted into the abdominal cavity. One or two additional trocars were placed (hybrid technique) to control
the pneumoperitoneum and to mobilize intrabdominal structures. Once the procedure was finished, the specimen
was retrieved through the vagina. Results: Eight procedures were performed using the previously described
techniques, including 3 cholecystectomies by TLS, 3 cholecystectomies by NOTES, 1 nephrectomy by TLS, and 1 nephrectomy
by NOTES, with mean operative time of 40.3, 63, 171.6 and 170 minutes, respectively. Difficulty in handling the
flexible endoscope in NOTES and intra and extra-abdominal instrument collision in TLS were the two intraoperative
incidents observed. Conclusions: These new techniques are feasible; however prospective clinical studies are still
necessary to confirm their real indications and benefits.
Key words: minimally invasive surgery, NOTES, transumbilical, cholecystectomy, nephrectomy.
Bras. J. Video-Sur, 2008, v. 1, n. 1: 029-036
| Accepted after revision: February, 07, 2008. |
INTRODUCTION
volution is part of Medicine; however, it is not
always easily accepted among physicians. In
the last decades surgical specialties have been experimenting advances and changes, thus even
more minimally invasive techniques have been adopted
to reduce patient's morbidity.
Since the initial description of a laparoscopic cholecystectomy in 1987 by
Mouret1 this evolution process has started. In spite of its steep learning
curve, different surgical specialties have already
adopted this minimally invasive approach as a
standard technique2-3, which resulted in reduced
postoperative pain, shorter hospital stay, earlier
postoperative recovery and better cosmetic
results4-8.
Recent laparoscopic surgical advances have been associated to the reduced size
and number of ports to reach the objective of a minimally invasive
surgery9-14. In the literature there are an increase number of reports
regarding the adoption of transumbilical approach
to perform cholecystectomies12,
oophorectomies13,
appendectomies14 and
nephrectomies9,10.
The most epic evolution of this continuous development process is the Natural
Orifice Transluminal Endoscopic Surgery (NOTES). It is
a new approach accessing without an incision the
abdominal cavity ("scarless surgery") having
natural orifices as the entry point to the abdomen,
i.e., transgatric, transvaginal, transvesical or
transcolonic access of the intra-abdominals organs through
the insertion of an endoscope into the peritoneal
cavity15. Therefore, without the incisions in the abdominal
wall surgical traumas would decrease even more. The
first report of this surgical technique was by Gettman
and cols. 16 in 2002, which depicted the feasibility
of transvaginal nephrectomies in an experimental
model at Texas University. Two years later, Kalloo e
cols. 17 performed transgastric hepatic biopsy at
Johns Hopkins University. After those initial reports
other researchers depicted the safety of transgastric
access to ligation of fallopian tubes18,
cholecystectomy19, cholecystogastric
anastomosis19,
gastrojejunostomy20, partial hysterectomy with
oophorectomy21,22,
splenectomy23, gastric
reduction24, nephrectomy25
and pancreatectomy26 , all of them based on
experimental studies in a porcine model. Since 2007, some
surgeons have performed
cholecystectomies27-32 and
nephrectomies33 by means of a transvaginal route
in human beings.
The objective of this manuscript is to present our clinical experience with these
new minimally invasive approaches.
PATIENTS AND METHODS
Instruments For Transumbilical Surgery
Basic laparoscopy instruments have been used to perform transumbilical surgeries.
Although some authors have already reported the use
of articulated laparoscopic10, staplers,
magnetic positioning of intra-abdominal cameras,
robotic prototypes11,34, in our experience the use of
these special instruments are not essential.
Surgical Team and Instruments for Notes
It is suggested that NOTES should be performed by a multidisciplinary team with at
least general surgeons and endoscopists, as it is a
surgical technique still being studied. A highly skilled team
in advanced laparoscopic surgery is required;
therefore in case of complications the surgery could be
promptly converted to laparoscopy.
The basic instruments to perform transluminal endoscopic surgeries include:
· double channel flexible endoscope (Karl Storz Endoskopi, Germany);
· hook knife (Olympus, Tokyo, Japan);
· needle knife (Olympus, Tokyo, Japan);
· hot biopsy forceps (Boston Scientific,
Natick, MA, USA);
· endoscopic clips (Clip Fixing Device, Olympus, Tokyo, Japan);
· grasping forceps (Olympus, Tokyo, Japan);
Transumbilical Access Surgical Technique
Patient should be placed in a position in the operating table accordingly to the surgical
procedure to be performed. After induction of
general anesthesia an oral-gastric tube is placed to
aspirate the stomach contents. Through the umbilicus
the Veress needle is inserted (Figure1A), thus
allowing the influx of carbon dioxide. Then
pneumoperitoneum is established and intra-abdominal pressure
is maintained between 12 and14 mmHg. A 10mm trocar for a
30o optic is inserted into the
periumbilical region, followed by two additional trocars (5mm
or 10mm) placed adjacent to the primary trocar. Therefore, we have two trocars to perform
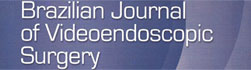
the planned procedure (Figures 1B, 1C e 2).
 |
Figure 1 - Transumbilical Laparoscopic Nephrectomy.
(A) Transumbilical Veress Needle placement for insufflation of
abdominal cavity. (B) Periumbilical trocars placement. (C)
External manipulation of instruments (D) Final aspect of the surgery. |
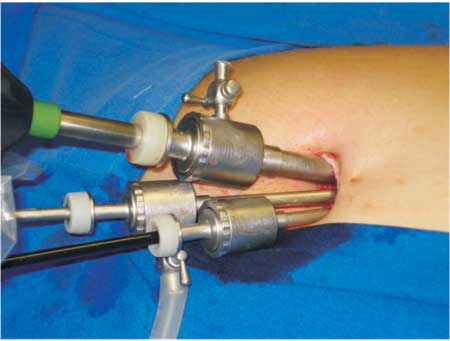 |
Figure 2 - Placement of trocars for transumbilical
laparoscopic cholecystectomy. |
At completion of the surgery, the specimen is placed into an endobag which is held with
a grasping forceps. The three trocars are removed
and the ports incisions are sutured (Figure 3A).
Then, the orifice in the aponeurosis is enlarged and
the endobag is easily retrieved from the abdominal cavity. In case of a cholecystectomy the
gallbladder is directly removed without the use of an
endobag (Figures 3B and 3C). Very large specimens
are removed by morcellation. Figures 1D and 3D depicted the surgery final aspect.
 |
Figure 3 - Transumbilical Laparoscopic Cholecystectomy.
(A) Approximation of the skin incision. (B e C) Gallbladder
removal through the umbilicus. (D) Final aspect of the
transumbilical incision in lambda form. |
Transvaginal Access Surgical Technique in Human Beings
Preoperative preparation of the patient
includes bowel preparation with fleet enema the night
before and 8 hours fasting. One hour prior to the surgery
vaginal embrocation with povidone-iodine is performed.
The procedure is performed under general anesthesia with patient placed in litothomy
position, legs supported by padded obstetric leg holders
and arms fastened along the body. Then, nasogastric
and vesical probe are placed. During the induction of
the anesthesia a prophylactic antibiotic (cefazoline 1g)
is administered. Povidine-iodine is used for cleansing
the operative field, and another vaginal embrocation
is performed with this solution.
A Sims speculum is inserted into the vagina and the cervix is grasped with a Pozzi forceps in
its posterior lip, then two Breisky retractors (one
posterior and one lateral) are used to expose the
structures. So, anterior traction of the cervix is performed to
stretch the posterior fornix, and the vaginal mucosa in
the posterior cul-de-sac is opened at the vaginal
cervix junction by a 2,5cm smile incision. After that, the
posterior margin is clamped with an Allis forceps and
with the index finger blunt dissection is
performed. Peritoneum of the posterior cul-de-sac is then
identified and opened.
Flexible endoscope is inserted into the peritoneal cavity and gas is insufflated to
establish pneumoperitoneum (Figure4A). A 5mm umbilical
trocar is used to control the abdominal pressure (12 a
14 mmHg) and to insert a clamp to mobilize the
abdominal structures (hybrid
technique)32. Another 5mm trocar may be placed depending on the
procedure33. (Figure 4D). Then proceed to endoscopic retro vision
to visualize the endoscope exact entry point in the
pouch of Douglas (Figure 4B). Then the endoscope is
moved forward into the abdominal cavity and
surgical procedure is performed (Figure 4C). At
completion of the surgery, the surgical specimen is retrieved
from the abdominal cavity with a polypectomy snare
(Figure 9) (Olympus, Tokyo, Japan).
 |
Figure 4 - Hybride Transvaginal NOTES. (A)
Laparoscopic visualization of the posterior cul-de-sac opening to vaginal
access in transvaginal hybrid nephrectomy. (B) View after
endoscope insertion through transvaginal route in transvaginal
hybrid cholecystectomy.(C) External manipulation of the endoscope
after insertion into the abdominal cavity. (D) Transvaginal
hybrid nephrectomy with two accessory ports. |
 |
Figure 9 - (A) Gallbladder removal with a polypectomy
snare after transvaginal hybrid cholecystectomy. (B) Kidney
prehension with polypectomy snare for retrieval from the abdominal
cavity after transvaginal hybrid nephrectomy. |
After reviewing the peritoneal cavity haemostasis, the pneumoperitoneum is deflated
and the cul-de-sac is closed with continuous suture of
2-0 chromic catgut or 2-0 vicryl.
RESULTS
From July 2007 until January 2008, one of the two approaches above described were performed
in eight patients submitted to surgery. Subsequently
we described the intraoperative details of each technique.
Transumbilical Approach
Until now we performed three transumbilical cholecystecytomy (Figures 5A,5B,5C e 5D) and
one transumbilical nephrectomy in our service. All cholecystectomis were performed with two 5
mm trocars (one to the optical trocar) and one 10mm
trocar. In fact, in the first case three trocars were
being used until the identification and isolation of artery
and the cystic duct; however, we had to substitute one
of the 5 mm trocar by a 10 mm due to technical
difficulties to place the clips using a 5mm clamp. Although
during 20 minutes we attempted to apply the 5mm
clamps, the operative time was 56 minutes. In the two
following cases a 10mm trocar was used since the beginning
of the surgery; therefore, the procedures last 30 and
35 minutes, respectively.
 |
Figure 5 - Transumbilical laparoscopic cholecystectomy.
(A) Release of the adhesions around the gallbladder (B) Cystic
duct dissection (C) Duct and cystic artery isolation. (D) Cystic
duct section after clips placement. |
There were no complications in the nephrectomy; thus special articulated
laparoscopic instruments were not necessary (Figure 6 and 7).
Two 5mm trocar and one 10 mm trocar for a 30o
optical were used. The procedure was performed in
63 minutes, and estimated bleeding was 50ml.
 |
Figure 6 - Transumbilical nephrectomy. (A) Colon
medial mobilization. (B e C) Identification and dissection of the
ureter. (D) Gonadal vein ligature. |
 |
Figure 7 - Transumbilical Laparoscopic Nephrectomy. (A)
Left renal artery ligation with Hem-o-lok. (B) Left renal vein
dissection. (C) Left renal vein ligation with Hem-o-lok. (D) Placement
of Hem-o-lok into the ureter. |
All postoperative patients had a good evolution, and they were discharged from hospital
on the first day after surgery.
Transvaginal Notes
Four patients were successfully submitted to transvaginal hybrid surgery, 3 cholecystectomies
and one nephrectomy.
In the cholecystectomies to control the pneumoperitoneum and the gallbladder mobilization
a 5mm transumbilical accessory puncture was performed. None of the cases presented
intra-operative bleeding (Figures 8A and 8B).
Incidents happened due to the inexperience in handling
the flexible endoscope to perform the surgery. The operative time of the three cholecystectomies
was 150,270 and 95 minutes, respectively. Patients did
not present any intraoperative complications and all
of them were discharged from hospital on the first postoperative day.
 |
Figure 8 - Hybrid transvaginal NOTES Cholecystectomy.
(A) Cystic duct dissection. (B) Dissection of the gallbladder from
the hepatic bed with a hook knife. |
Two 5mm abdominal accessory trocars were placed, one transumbilical and another
subxiphoid during nephrectomy. Operative time was 170
minutes and estimated bleeding was 350ml.
On the morning day after surgery four patients received a regular diet and on the
first postoperative day they were discharged from
hospital. Analgesia required only ordinary
analgesic (dipirone) to relieve pain in all cases.
Postoperatively patients were oriented to restart sexual activity after 40 days.
DISCUSSION
With the advent and rapid revolutionary evolution of laparoscopic surgery all over
the world in 1990's decade, unquestionable
advantages over open surgery are evident: as less postoperative pain, cosmetic surgery, short
length of hospital stay, quick pulmonary recovery
and prompt return to work.
Nevertheless, experimental and clinical researches are still searching for new
minimally invasive surgical techniques and approaches.
New procedures to improve postoperative recovery
and reduce risks have been arising everyday in the
world literature as a way to overcome the
laparoscopic approaches results.
Enlargement of port site or an additional port is frequently necessary to remove
specimen. Depending on the procedure performed at
surgery completion patients usually have 3 to 6 incisions
about 1 to 4 centimeters long. Laparoscopy incisions
potential morbidity include: worst cosmetic results,
cutaneous innervations injury, chronic pain, subcutaneous
bleeding and development of incisional
hernia10.
In order to spare patients from morbidity associated to incisions, some techniques such
as morcellation, transvaginal extraction of the
surgical specimen, natural orifices surgery and
transumbilical surgery have been developed to reduce the
number of incisions and/or remove the surgical specimen
after laparoscopic procedure.
As a way to reduce the above mentioned
morbidity35-40 morcellation of specimens have
been performed in some institutions; however, this
approach has a negative impact as the specimen can not
be evaluated for pathological staging41, limiting its use
with malignant tumors.
Traditionally gynecologists used transvaginal route to performed procedures such
as hysterectomies42,
adnexectomy43, tubal
ligation44 and others. In addition to that many authors have
already described vaginal removal of surgical specimens
after gynecological laparoscopies45-49
. Transvaginal access has already been used to remove surgical
specimens after laparoscopic procedures even by some
general surgeons and urologists. Extraction of
surgical specimens from the abdominal cavity is a
feasible approach; however unfortunately it can only
be performed in female patients.
Recently, the Natural Orifice Transluminal Endoscopic Surgery (NOTES) - a new
revolutionary concept of minimally invasive surgery has
attracted surgeons and endoscopists. The three
main justifications for NOTES are improved
cosmetic appearance, easy access, and the concept that
human ability and technological advance can continue
to reduce patients' trauma and discomfort, and
maintain surgery effectiveness 55.
NOTES is a less invasive procedure as well as laparoscopy; therefore it is an alternative
technique to open surgery as it can reduce postoperative
stress, morbidity and hospital length stay. Moreover,
NOTES has a theoretically potential to reduce risk
of complications such as wounds infections,
postoperative hernia and adhesions17-19. An additional advantage
of this approach is that it could be performed in
patients with extensive scars, serious burns, infection of
the abdominal wall and morbid obesity, besides the
high risk and critically ill patients56. In this manuscript
we report four successful cases of hybrid
transvaginal NOTES. Difficulty in handling the flexible
endoscope and manipulating instruments to perform basic
surgical maneuvers can be explained by our
procedures operative time. Although we believe learning
curve data should be evaluated as it is in laparoscopy;
due to our small sample it was not possible to be
evaluated. In our opinion, transvaginal endoscopic
surgery benefits are scientifically acknowledged, thus it
will not cause an additional risk of postoperative
fistulae in patients (transgastric, transcolonic and
transvesical access).
Transumbilical surgery is an alternative technique to traditional laparoscopy with an
improved cosmetic result due to the periumbilical
incision. Moreover, comparing to NOTES it has a short
learning curve because the anatomic visualization is almost
the same to the traditional laparoscopy what changes
is the puncture site10. The four reported cases
were successfully performed without difficulties. As
trocars were placed into the periumblical region, they
were jointed through elliptical incision to remove the
surgical specimen. As we did not have any
articulated instrument intra and extra-abdominal collision
were the only intraoperative incident regarding trocars.
One kidney and three gallbladders were removed from
the abdominal cavity, without morcellation.
CONCLUSIONS
Any new technology should be carefully used with human beings. Until the present moment only a few cases were reported in the literature. The development of new endoscopic tools and accessories certainly will accelerate the development of NOTES technique and improve its results; therefore in the future it may become an acceptable alternative technique and a preferable access route for some special abdominopelvic conditions in well selected patients. Transumbilical laparoscopic surgery is a feasible technique, as it is similar to traditional laparoscopy, except for the position of the trocars. Proposed benefits and safety of both surgical techniques still need to be depicted in further clinical studies comparing the two techniques to traditional techniques.
REFERENCES
1. Mouret P. From the first laparoscopic cholecystectomy
to the frontiers of laparoscopic surgery; the future
prospective. Dig Surg 1991; 8: 124-5.
2. Kondo W, Garcia MJ, Ivano FH, Bahten LCV, Miyake
RT, Smaniotto B. Curva de aprendizado na
fundoplicatura laparoscópica durante a residência médica em cirurgia
geral. Rev Col Bras Cir 2006; 33: 96-100.
3. Peterli R, Herzog U, Schuppisser JP, Ackermann C,
Tondelli P. The learning curve of laparoscopic cholecystectomy
and changes in indications: one institutions's experience
with 2,650 cholecystectomies. J Laparoendosc Adv Surg Tech
A 2000; 10: 13-9.
4. Branco AW, Branco Filho AJ, Kondo W, George MA,
Maciel RF, Garcia MJ. Hand-assisted right laparoscopic live
donor nephrectomy. Int Braz J Urol 2005; 31: 421-9.
5. Kondo W, Rangel M, Tirapelle RA, Garcia MJ, Bahten
LCV, Laux GL, et al. Emprego da laparoscopia em mulheres
com dor abdominal aguda. Rev Bras Videocir 2006; 4: 3-8.
6. Ortega AE, Hunter JG, Peters JH, Swanstrom LL,
Schirmer B. A prospective, randomized comparison of
laparoscopic appendectomy with open appendectomy.
Laparoscopic Appendectomy Study Group. Am J Surg 1995; 169:
208-12.
7. Schauer PR, Ikramuddin S. Laparoscopic surgery for
morbid obesity. Surg Clin North Am 2001; 81: 1145-79.
8. Topçu O, Karakayali F, Kuzu MA, Ozdemir S, Erverdi
N, Elhan A, et al. Comparison of long-term quality of life
after laparoscopic and open cholecystectomy. Surg Endosc
2003; 17: 291-5.
9. Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai
MR, Mishra S, et al. Scarless single port
transumbilical nephrectomy and pyeloplasty: first clinical report. BJU
Int 2008; 101: 83-8.
10. Raman JD, Bensalah K, Bagrodia A, Stern JM, Cadeddu
JA. Laboratory and clinical development of single keyhole
umbilical nephrectomy. Urology 2007; 70: 1039-42.
11. Zeltser IS, Bergs R, Fernandez R, Baker L, Eberhart
R, Cadeddu JA. Single trocar laparoscopic nephrectomy
using magnetic anchoring and guidance system in the porcine
model. J Urol 2007; 178: 288-91.
12. Cuesta MA, Berends F, Veenhof AA. The
"invisible cholecystectomy": A transumbilical laparoscopic
operation without a scar. Surg Endosc 2007; Oct 18.
13. Lin JY, Lee ZF, Chang YT. Transumbilical management
for neonatal ovarian cysts. J Pediatr Surg 2007; 42: 2136-9.
14. Martínez AP, Bermejo MA, Cortœ JC, Orayen CG,
Chacón JP, Bravo LB. Appendectomy with a single trocar
through the umbilicus: results of our series and a cost
approximation. Cir Pediatr 2007; 20: 10-4.
15. de la Fuente SG, Demaria EJ, Reynolds JD, Portenier
DD, Pryor AD. New developments in surgery: Natural
Orifice Transluminal Endoscopic Surgery (NOTES). Arch Surg
2007; 142: 295-7.
16. Gettman MT, Lotan Y, Napper CA, Cadeddu
JA. Transvaginal laparoscopic nephrectomy: development
and feasibility in the porcine model. Urology 2002; 59: 446-50.
17. Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill
SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: a
novel approach to diagnostic and therapeutic interventions in
the peritoneal cavity. Gastrointest Endosc 2004; 60: 114-7.
18. Jagannath SB, Kantsevoy SV, Vaughn CA, Chung SS,
Cotton PB, Gostout CJ, et al. Peroral transgastric endoscopic
ligation of fallopian tubes with long-term survival in a porcine
model. Gastrointest Endosc 2005; 61: 449-53.
19. Park PO, Bergström M, Ikeda K, Fritscher-Ravens A,
Swain P. Experimental studies of transgastric gallbladder
surgery: cholecystectomy and cholecystogastric anastomosis
(videos). Gastrointest Endosc 2005; 61: 601-6.
20. Kantsevoy SV, Jagannath SB, Niiyama H, Chung SS,
Cotton PB, Gostout CJ, et al. Endoscopic gastrojejunostomy
with survival in a porcine model. Gastrointest Endosc 2005;
62: 287-92.
21. Wagh MS, Merrifield BF, Thompson CC.
Endoscopic transgastric abdominal exploration and organ resection:
initial experience in a porcine model. Clin Gastroenterol
Hepatol 2005; 3: 892-6.
22. Wagh MS, Merrifield BF, Thompson CC. Survival
studies after endoscopic transgastric oophorectomy and
tubectomy in a porcine model. Gastrointest Endosc 2006; 63: 473-8.
23. Kantsevoy SV, Hu B, Jagannath SB, Vaughn CA,
Beitler DM, Chung SS, et al. Transgastric endoscopic
splenectomy: is it possible? Surg Endosc 2006; 20: 522-5.
24. Kantsevoy SV, Hu B, Jagannath SB, Isakovich NV,
Chung SS, Cotton PB, et al. Technical feasibility of
endoscopic gastric reduction: a pilot study in a porcine
model. Gastrointest Endosc 2007; 65: 510-3.
25. Lima E, Rolanda C, Pêgo JM, Henriques-Coelho T, Silva
D, Osório L, et al. Third-generation nephrectomy by
natural orifice transluminal endoscopic surgery. J Urol 2007;
178: 2648-54.
26. Matthes K, Yusuf TE, Willingham FF, Mino-Kenudson
M, Rattner DW, Brugge WR. Feasibility of
endoscopic transgastric distal pancreatectomy in a porcine animal
model. Gastrointest Endosc. 2007 Oct;66(4):762-6.
27. Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter
D, Coumaros D. Surgery without scars: report of
transluminal cholecystectomy in a human being. Arch Surg 2007; 142: 823-6.
28. Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho
GL, Filgueiras M. NOTES transvaginal
cholecystectomy: preliminary clinical application. Surg Endosc 2008; 22: 542-7.
29. Zorrón R, Filgueiras M, Maggioni LC, Pombo L,
Lopes Carvalho G, Lacerda Oliveira A. NOTES.
Transvaginal cholecystectomy: report of the first case. Surg Innov
2007; 14: 279-83.
30. Zornig C, Emmermann A, von Waldenfels HA, Mofid
H. Laparoscopic cholecystectomy without visible
scar: combined transvaginal and transumbilical
approach. Endoscopy 2007; 39: 913-5.
31. Bessler M, Stevens PD, Milone L, Parikh M, Fowler
D. Transvaginal laparoscopically assisted
endoscopic cholecystectomy: a hybrid approach to natural
orifice surgery. Gastrointest Endosc 2007; 66: 1243-5.
32. Branco Filho AJ, Noda RW, Kondo W, Kawahara
N, Rangel M, Branco AW. Initial experience with
hybrid transvaginal cholecystectomy. Gastrointest Endosc
2007; 66: 1245-8.
33. Branco AW, Filho AJ, Kondo W, Noda RW, Kawahara
N, Camargo AA, et al. Hybrid Transvaginal Nephrectomy.
Eur Urol 2007; Nov 5.
34. Park S, Bergs RA, Eberhart R, Baker L, Fernandez R,
Cadeddu JA. Trocar-less instrumentation for laparoscopy:
magnetic positioning of intra-abdominal camera and retractor. Ann
Surg 2007; 245: 379-84.
35. Urban DA, Kerbl K, McDougall EM, Stone AM,
Fadden PT, Clayman RV. Organ entrapment and renal
morcellation: permeability studies. J Urol 1993; 150: 1792-4.
36. Landman J, Venkatesh R, Kibel A, Vanlangendonck
R. Modified renal morcellation for renal cell
carcinoma: laboratory experience and early clinical application.
Urology 2003; 62: 632-4.
37. Camargo AH, Rubenstein JN, Ershoff BD, Meng MV,
Kane CJ, Stoller ML. The effect of kidney morcellation
on operative time, incision complications, and
postoperative analgesia after laparoscopic nephrectomy. Int Braz J
Urol 2006; 32: 273-9.
38. Varkarakis I, Rha K, Hernandez F, Kavoussi LR,
Jarrett TW. Laparoscopic specimen extraction: morcellation.
BJU Int 2005; 95: 27-31.
39. Greene AK, Hodin RA. Laparoscopic splenectomy for
massive splenomegaly using a Lahey bag. Am J Surg 2001; 181:
543-6.
40. Bojahr B, Raatz D, Schonleber G, Abri C, Ohlinger
R. Perioperative complication rate in 1706 patients after
a standardized laparoscopic supracervical
hysterectomy technique. J Minim Invasive Gynecol 2006; 13: 183-9.
41. Kaouk JH, Gill IS. Laparoscopic radical
nephrectomy: morcellate or leave intact? Leave intact. Rev Urol 2002;
4: 38-42.
42. Figueiredo O, Figueiredo EG, Figueiredo PG, Pelosi
MA 3rd, Pelosi MA. Vaginal removal of the benign
nonprolapsed uterus: experience with 300 consecutive operations.
Obstet Gynecol 1999; 94: 348-51.
43. Sahin Y. Vaginal hysterectomy and oophorectomy in
women with 12-20 weeks' size uterus. Acta Obstet Gynecol
Scand 2007; 86: 1359-69.
44. Hartfield VJ. Female sterilization by the vaginal route:
a positive reassessment and comparison of 4 tubal
occlusion methods. Aust N Z J Obstet Gynaecol 1993; 33:408-12.
45. Blecharz A, Rzempo³uch J, Zam³yñski J.
Laparoscopic hysterectomy with vaginal extraction. Ginekol Pol 1994;
65: 477-81.
46. Ghezzi F, Raio L, Mueller MD, Gyr T, Buttarelli M,
Franchi M. Vaginal extraction of pelvic masses following
operative laparoscopy. Surg Endosc 2002; 16: 1691-6.
47. Jadoul P, Feyaerts A, Squifflet J, Donnez J.
Combined laparoscopic and vaginal approach for
nephrectomy, ureterectomy, and removal of a large
rectovaginal endometriotic nodule causing loss of renal function. J
Minim Invasive Gynecol 2007; 14: 256-9.
48. Pardi G, Carminati R, Ferrari MM, Ferrazzi E, Bulfoni
G, Marcozzi S. Laparoscopically assisted vaginal removal
of ovarian dermoid cysts. Obstet Gynecol 1995; 85: 129-32.
49. Spuhler SC, Sauthier PG, Chardonnens EG, De Grandi P.
A new vaginal extractor for laparoscopic surgery. J Am
Assoc Gynecol Laparosc 1994; 1: 401-4.
50. Breitenstein S, Dedes KJ, Bramkamp M, Hess T,
Decurtins M, Clavien PA. Synchronous laparoscopic sigmoid
resection and hysterectomy with transvaginal specimen removal.
J Laparoendosc Adv Surg Tech A 2006; 16: 286-9.
51. Vereczkei A, Illenyi L, Arany A, Szabo Z, Toth L,
Horváth OP. Transvaginal extraction of the laparoscopically
removed spleen. Surg Endosc 2003; 17: 157.
52. Zornig C, Emmermann A, von Waldenfels HA,
Felixmüller C. Colpotomy for specimen removal in laparoscopic
surgery. Chirurg 1994; 65: 883-5.
53. Gill IS, Cherullo EE, Meraney AM, Borsuk F, Murphy
DP, Falcone T. Vaginal extraction of the intact specimen
following laparoscopic radical nephrectomy. J Urol 2002; 167:
238-41.
54. Yuan LH, Chung HJ, Chen KK. Laparoscopic
radical cystectomy combined with bilateral nephroureterectomy
and specimen extraction through the vagina. J Chin Med
Assoc 2007; 70: 260-1.
55. Swain P. A justification for NOTES _ natural
orifice translumenal endosurgery. Gastrointest Endosc 2007;
65: 514-6.
56. Inui K. Natural orifice transluminal endoscopic surgery:
a step toward clinical implementation? Gastrointest
Endosc 2007; 65: 694-5.
Correspondence address:
William Kondo
Address: Av. Getúlio Vargas, 3163 ap. 21
CEP 80240-041
Curitiba - Paraná
E-mail: williamkondo@yahoo.com